A stroke occurs when the blood supply to part of your brain is interrupted or severely reduced, depriving brain tissue of oxygen and nutrients. Within minutes, brain cells begin to die. A stroke is a medical emergency. Prompt treatment is crucial. Early action can minimize brain damage and potential complications. The good news is that strokes can be treated and prevented, and many fewer Americans die of stroke now than even 15 years ago.
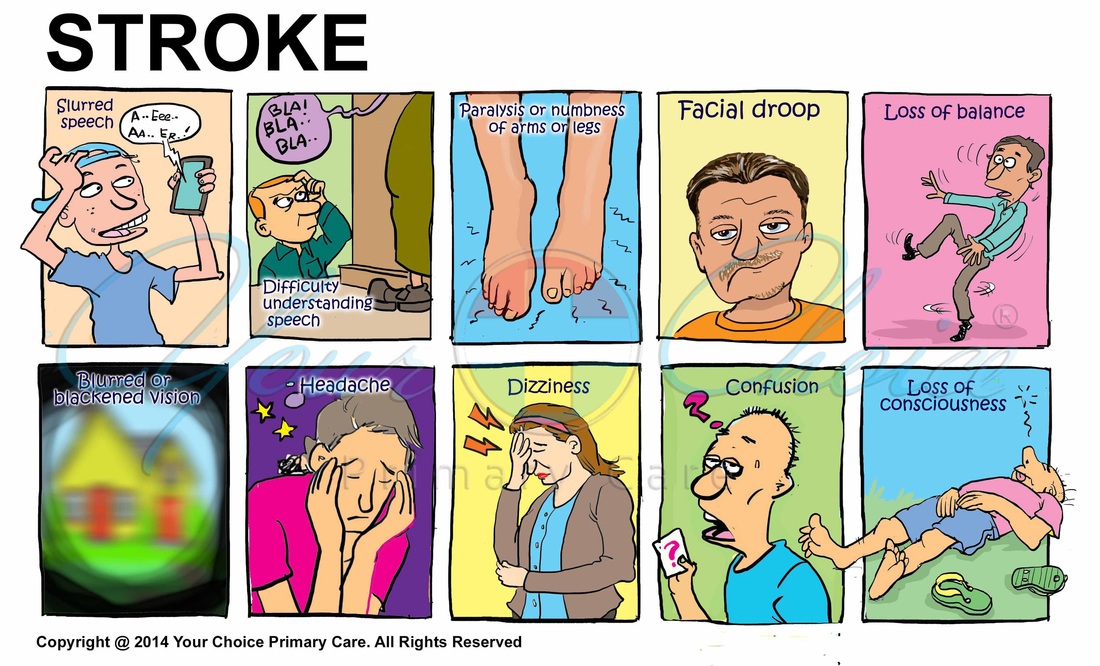
Watch for these signs and symptoms if you think you or someone else may be having a stroke. Note when your signs and symptoms begin, because the length of time they have been present may guide your treatment decisions:
- Trouble with speaking and understanding. You may experience confusion. You may slur your words or have difficulty understanding speech.
- Paralysis or numbness of the face, arm or leg. You may develop sudden numbness, weakness or paralysis in your face, arm or leg, especially on one side of your body. Try to raise both your arms over your head at the same time. If one arm begins to fall, you may be having a stroke. Similarly, one side of your mouth may droop when you try to smile.
- Trouble with seeing in one or both eyes. You may suddenly have blurred or blackened vision in one or both eyes, or you may see double.
- Headache. A sudden, severe headache, which may be accompanied by vomiting, dizziness or altered consciousness, may indicate you're having a stroke.
- Trouble with walking. You may stumble or experience sudden dizziness, loss of balance or loss of coordination.
When to see a doctor
Seek immediate medical attention if you notice any signs or symptoms of a stroke, even if they seem to fluctuate or disappear. Call 911 or your local emergency number right away. Don't wait to see if symptoms go away. Every minute counts. The longer a stroke goes untreated, the greater the potential for brain damage and disability.
A stroke occurs when the blood supply to your brain is interrupted or reduced. This deprives your brain of oxygen and nutrients, which can cause your brain cells to die.
Ischemic strokes occur when the arteries to your brain become narrowed or blocked, causing severely reduced blood flow (ischemia). The most common ischemic strokes include:
- Thrombotic stroke. A thrombotic stroke occurs when a blood clot (thrombus) forms in one of the arteries that supply blood to your brain. A clot may be caused by fatty deposits (plaque) that build up in arteries and cause reduced blood flow (atherosclerosis) or other artery conditions.
- Embolic stroke. An embolic stroke occurs when a blood clot or other debris forms away from your brain — commonly in your heart — and is swept through your bloodstream to lodge in narrower brain arteries. This type of blood clot is called an embolus.
Hemorrhagic stroke occurs when a blood vessel in your brain leaks or ruptures. Brain hemorrhages can result from many conditions that affect your blood vessels, including uncontrolled high blood pressure, and weak spots in your blood vessel walls (aneurysms). A less common cause of hemorrhage is the rupture of an abnormal tangle of thin-walled blood vessels (arteriovenous malformation) present at birth.
A transient ischemic attack (TIA) — also known as a ministroke — is a brief period of symptoms similar to those you'd have in a stroke. A temporary decrease in blood supply to part of your brain causes TIAs. Like an ischemic stroke, a TIA occurs when a clot or debris blocks blood flow to part of your brain. A TIA doesn't leave lasting symptoms because the blockage is temporary.
Seek emergency care even if your symptoms seem to clear up. Having a TIA puts you at greater risk of having a full-blown stroke, causing permanent damage later. If you've had a TIA, it means there's likely a partially blocked or narrowed artery leading to your brain or a clot source in the heart. It's not possible to tell if you're having a stroke or a TIA based only on your symptoms. Up to half of people whose symptoms appear to go away actually have had a stroke causing brain damage.
Many factors can increase your risk of a stroke. Some factors can also increase your chances of having a heart attack. Potentially treatable stroke risk factors include:
- Being overweight or obese
- Physical inactivity
- Heavy or binge drinking
- Use of illicit drugs such as cocaine and methamphetamines
- High blood pressure — the risk of stroke begins to increase at blood pressure readings higher than 120/80 millimeters of mercury (mm Hg). Your doctor will help you decide on a target blood pressure based on your age, whether you have diabetes and other factors.
- Cigarette smoking or exposure to secondhand smoke.
- High cholesterol.
- Diabetes.
- Obstructive sleep apnea — a sleep disorder in which the oxygen level intermittently drops during the night.
- Cardiovascular disease, including heart failure, heart defects, heart infection or abnormal heart rhythm.
- Personal or family history of stroke, heart attack or transient ischemic attack.
- Being age 55 or older.
- Race — African-Americans have a higher risk of stroke than do people of other races.
- Gender — Men have a higher risk of stroke than women. Women are usually older when they have strokes, and they're more likely to die of strokes than are men. Also, they may have some risk from some birth control pills or hormone therapies that include estrogen.
A stroke can sometimes cause temporary or permanent disabilities, depending on how long the brain lacks blood flow and which part was affected. Complications may include:
- Paralysis or loss of muscle movement. You may become paralyzed on one side of your body, or lose control of certain muscles, such as those on one side of your face or one arm. Physical therapy may help you return to activities hampered by paralysis, such as walking, eating and dressing.
- Difficulty talking or swallowing. A stroke may cause you to have less control over the way the muscles in your mouth and throat move, making it difficult for you to talk clearly (dysarthria), swallow or eat (dysphagia). You also may have difficulty with language (aphasia), including speaking or understanding speech, reading or writing. Therapy with a speech and language pathologist may help.
- Memory loss or thinking difficulties. Many people who have had strokes experience some memory loss. Others may have difficulty thinking, making judgments, reasoning and understanding concepts.
- Emotional problems. People who have had strokes may have more difficulty controlling their emotions, or they may develop depression.
- Pain. People who have had strokes may have pain, numbness or other strange sensations in parts of their bodies affected by stroke.
- Changes in behavior and self-care ability. People who have had strokes may become more withdrawn and less social or more impulsive. They may need help with grooming and daily chores.
Most stroke survivors receive treatment in a rehabilitation program. Your doctor will recommend the most rigorous therapy program you can handle based on your age, overall health and your degree of disability from your stroke. Your doctor will take into consideration your lifestyle, interests and priorities, and the availability of family members or other caregivers. Your rehabilitation program may begin before you leave the hospital. It may continue in a rehabilitation unit of the same hospital, another rehabilitation unit or skilled nursing facility, an outpatient unit, or your home.
A stroke is a life-changing event that can affect your emotional well-being as much as your physical function. You may experience feelings of helplessness, frustration, depression and apathy. You may also have mood changes and less of a sex drive. Maintaining your self-esteem, connections to others and interest in the world are essential parts of your recovery. Several strategies may help you and your caregivers, including:
- Don't be hard on yourself. Accept that physical and emotional recovery will involve tough work and that it will take time. Aim for a "new normal," and celebrate your progress. Allow time for rest.
- Get out of the house even if it's hard. Try not to be discouraged or self-conscious if you move slowly and need a cane, walker or wheelchair to get around. Getting out is good for you.
- Join a support group. Meeting with others who are coping with a stroke lets you get out and share experiences, exchange information and forge new friendships.
- Let friends and family know what you need. People may want to help, but they may not know what to do. Let them know how they can help, such as by bringing over a meal and staying to eat with you and talk, or attending social events or religious activities.
- Know that you are not alone. Nearly 800,000 Americans have a stroke every year. Approximately every 40 seconds someone has a stroke in the United States.
- Practice will help. Try to have a conversation at least once a day. It will help you learn what works best for you, feel connected and rebuild your confidence.
- Relax and take your time. Talking may be easiest and most enjoyable in a relaxing situation when you have plenty of time. Some stroke survivors find that after dinner is a good time.
- Say it your way. When you're recovering from a stroke, you may need to use fewer words, rely on gestures or use your tone of voice to communicate.
- Use props and communication aids. You may find it helpful to use cue cards showing frequently used words, pictures of close friends and family members, or daily activities, such as a favorite television show or the bathroom.
Many stroke prevention strategies are the same as strategies to prevent heart disease. In general, healthy lifestyle recommendations include:
- Controlling high blood pressure (hypertension). One of the most important things you can do to reduce your stroke risk is to keep your blood pressure under control. If you've had a stroke, lowering your blood pressure can help prevent a subsequent transient ischemic attack or stroke. Exercising, managing stress, maintaining a healthy weight, and limiting the amount of sodium and alcohol you eat and drink are all ways to keep high blood pressure in check.. In addition to recommending lifestyle changes, your doctor may prescribe medications to treat high blood pressure.
- Lowering the amount of cholesterol and saturated fat in your diet. Eating less cholesterol and fat, especially saturated fat and trans fats, may reduce the fatty deposits (plaques) in your arteries. If you can't control your cholesterol through dietary changes alone, your doctor may prescribe a cholesterol-lowering medication.
- Quitting tobacco use. Smoking raises the risk of stroke for smokers and nonsmokers exposed to secondhand smoke. Quitting tobacco use reduces your risk of stroke.
- Controlling diabetes. You can manage diabetes with diet, exercise, weight control and medication.
- Maintaining a healthy weight. Being overweight contributes to other stroke risk factors, such as high blood pressure, cardiovascular disease and diabetes. Weight loss of as little as 10 pounds may lower your blood pressure and improve your cholesterol levels.
- Eating a diet rich in fruits and vegetables. A diet containing five or more daily servings of fruits or vegetables may reduce your risk of stroke. Following the Mediterranean diet, which emphasizes olive oil, fruit, nuts, vegetables and whole grains, may be helpful.
- Exercising regularly. Aerobic or "cardio" exercise reduces your risk of stroke in many ways. Exercise can lower your blood pressure, increase your level of high-density lipoprotein cholesterol, and improve the overall health of your blood vessels and heart. It also helps you lose weight, control diabetes and reduce stress. Gradually work up to 30 minutes of activity — such as walking, jogging, swimming or bicycling — on most, if not all, days of the week.
- Drinking alcohol in moderation, if at all. Alcohol can be both a risk factor and a protective measure for stroke. Heavy alcohol consumption increases your risk of high blood pressure, ischemic strokes and hemorrhagic strokes.
- Treating obstructive sleep apnea, if present. Your doctor may recommend an overnight oxygen assessment to screen for obstructive sleep apnea (OSA). If OSA is detected, it may be treated by giving you oxygen at night or having you wear a small device in your mouth.
- Avoiding illicit drugs. Certain street drugs, such as cocaine and methamphetamines, are established risk factors for a TIA or a stroke. Cocaine reduces blood flow and can cause narrowing of arteries.
If you've had an ischemic stroke or TIA, your doctor may recommend medications to help reduce your risk of having another stroke. These include:
- Anti-platelet drugs. Platelets are cells in your blood that initiate clots. Anti-platelet drugs make these cells less sticky and less likely to clot. The most commonly used anti-platelet medication is aspirin. Your doctor may also consider prescribing Aggrenox, a combination of low-dose aspirin and the anti-platelet drug dipyridamole, to reduce the risk of blood clotting. If aspirin doesn't prevent your TIA or stroke, or if you can't take aspirin, your doctor may instead prescribe an anti-platelet drug such as clopidogrel (Plavix).
- Anticoagulants. These drugs, which include heparin and warfarin (Coumadin), reduce blood clotting. Your doctor may prescribe these drugs if you have certain blood-clotting disorders, certain arterial abnormalities, an abnormal heart rhythm or other heart problems.