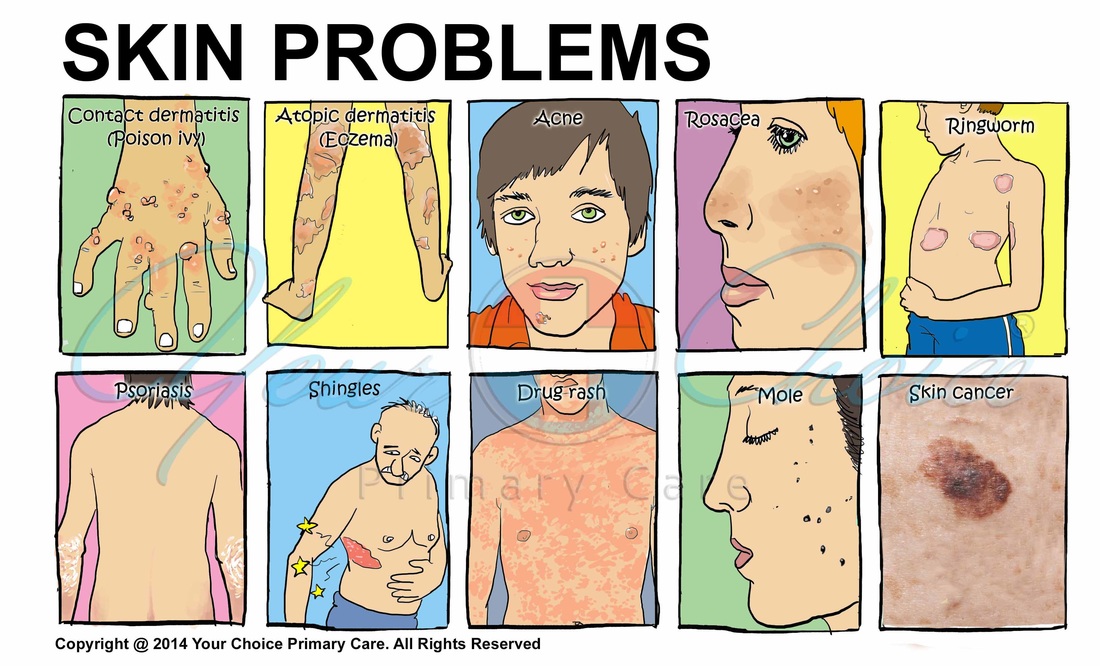
Skin Problems
- Contact Dermatitis (poison ivy, poison oak)
- Atopic Dermatitis (eczema)
- Acne
- Rosacea
- Ringworm
- Psoriasis
- Shingles
- Mole
- Skin Cancer
<Contact Dermatitis>
Contact dermatitis is a red, itchy rash caused by a substance that comes into contact with your skin. The rash isn't contagious or life-threatening, but it can be very uncomfortable.
Possible causes include soaps, cosmetics, fragrances, jewelry, and plants, such as poison ivy or poison oak. Some people are exposed to substances at work that may cause contact dermatitis.
To treat contact dermatitis successfully, you need to identify and avoid the cause of your reaction. If you can avoid the offending substance, the rash usually clears up in two to four weeks. You can try soothing your skin with cool, wet compresses, and anti-itch creams.
Contact dermatitis usually occurs on areas of your body that have been directly exposed to the substance — for example, along a calf that brushed against poison ivy or under a watchband that triggers an allergy. The reaction usually develops within minutes to hours of exposure to an irritating substance or allergen. The rash can last two to four weeks.
Signs and symptoms of contact dermatitis include:
- Red rash or bumps
- Itching, which may be severe
- Dry, cracked, scaly skin
- Blisters, draining fluid and crusting
- Swelling, burning or tenderness
The severity of the rash depends on:
- How long you're exposed
- The strength of the substance that caused the rash
- Environmental factors, such as temperature, airflow and sweating from wearing gloves
- Your genetic makeup, which can affect how you respond to certain substances
When to see a doctor
See your doctor if:
- The rash is so uncomfortable that you are losing sleep or are distracted from your daily routine
- The rash is painful, severe or widespread
- You're embarrassed by the way your skin looks
- The rash doesn't get better within a few weeks
- The rash affects your face or genitals
Seek immediate medical care in the following situations:
- You think your skin is infected — clues include fever and pus oozing from blisters.
- Your lungs, eyes or nasal passages are painful and inflamed, perhaps from inhaling an allergen.
- You think the rash has damaged the mucous lining of your mouth and digestive tract.
Contact dermatitis is caused by a substance you're exposed to that irritates your skin or triggers an allergic reaction. The substance could be one of thousands of known allergens and irritants. Some of these substances may cause both irritant contact dermatitis and allergic contact dermatitis.
Irritant contact dermatitis is the most common type. This nonallergic inflammatory reaction occurs when a substance damages your skin's outer protective layer.
Some people react to strong irritants after a single exposure. Others may develop signs and symptoms after repeated exposures to even mild irritants. And some people develop a tolerance to the substance over time.
Common irritants include:
- Solvents
- Rubbing alcohol
- Bleach
- Personal care products, such as soaps, deodorants and cosmetics
- Airborne substances, such as sawdust or wool dust
- Burdock, a plant used in alternative medicine therapies
Allergic contact dermatitis occurs when a substance to which you're sensitive (allergen) triggers an immune reaction in your skin. It usually affects only the area that came into contact with the allergen. But it may be triggered by something that enters your body through foods. You may become sensitized to a strong allergen such as poison ivy after a single exposure. Weaker allergens may require multiple exposures over several years to trigger an allergy. Once you develop an allergy to a substance, even a small amount of it can cause a reaction.
Common allergens include:
- Nickel, which is used in jewelry, buckles and many other items
- Balsam of Peru, which is used in many products, such as perfumes, cosmetics, mouth rinses and flavorings
- Formaldehyde, which is in adhesives, solvents and many other things
- Personal care products, such as deodorants, body washes, hair dyes, cosmetics, nail polish
- Herbal preparations for the skin containing eucalyptus, camphor or rosemary
- Skin tattooing and black henna
- Plants such as poison ivy and mango, which contain a highly allergenic substance called urushiol
- Airborne substances, such as from aromatherapy and spray insecticides
- Products that cause a reaction when you're in the sun (photoallergic contact dermatitis), such as some sunscreens
Occupational contact dermatitis refers to rashes resulting from exposure to allergens or irritants on the job. Certain occupations and hobbies put you at higher risk of this type of contact dermatitis.
Examples include:
- Health care workers and pharmaceutical industry employees
- Metalworkers
- Construction workers
- Hairdressers and cosmetologists
- Waiters
- Scuba divers or swimmers, due to the rubber in face masks or goggles
- Cleaners
- Gardeners and agricultural workers
- Chefs and others who work with food
You're likely to start by seeing your primary care doctor. He or she might refer you to a doctor who specializes in skin disorders (dermatologist).
The key to successful treatment of contact dermatitis is identifying what's causing your symptoms and figuring out whether you have the irritant or allergic type. Doctors rely on these main steps to determine the cause:
- A thorough medical history and physical exam. Your doctor may be able to diagnose contact dermatitis and identify its cause by talking to you about your signs and symptoms, questioning you to uncover clues about the culprit, and examining your skin to note the pattern and intensity of your reaction.
- An allergy test. Your doctor may recommend a test to see if you're allergic to something. This test can be useful if the cause of your rash isn't apparent or if your rash recurs often.
- Avoiding the irritant or allergen. The key to this is identifying what's causing your rash and then staying away from it.
- Applying prescription steroid creams. If self-care measures haven't worked, your doctor may prescribe a steroid cream.
- Using oral medications. In severe cases, your doctor may prescribe oral corticosteroids to reduce inflammation, antihistamines to relieve itching or antibiotics to fight a bacterial infection.
To help reduce itching and soothe inflamed skin, try these self-care approaches:
- Avoid allowing the reaction-causing substance to touch your skin. If it's a piece of jewelry, you may be able to wear it by putting a barrier between you and the metal. For example, line the inside of a bracelet with a piece of clear tape or paint it with clear nail polish.
- Apply an anti-itch cream or calamine lotion to the affected area. A nonprescription cream containing at least 1 percent hydrocortisone can temporarily relieve your itch.
- Take an over-the-counter anti-itch drug. A nonprescription oral antihistamine, such as diphenhydramine (Benadryl, others), may be helpful if your itching is severe.
- Apply cool, wet compresses. Moisten soft washcloths and hold them against the rash to soothe your skin for 15 to 30 minutes. Repeat several times a day.
- Avoid scratching. Trim your nails. If you can't keep from scratching an itchy area, cover it with a dressing and bandage.
- Soak in a comfortably cool bath. Sprinkle the water with baking soda or an oatmeal-based bath product (Aveeno, others).
- Wear smooth-textured cotton clothing. This helps avoid irritation.
- Choose mild soaps without dyes or perfumes. Rinse completely, pat your skin dry and apply moisturizer.
- Protect your hands with moisturizers and gloves. Reapply moisturizers throughout the day. And choose gloves based on what you're protecting your hands from. For example, plastic gloves lined with cotton are good if your hands are often wet.
<Atopic dermatitis>
Atopic dermatitis (eczema) is a condition that makes your skin red and itchy. It's common in children but can occur at any age. Atopic dermatitis is long lasting (chronic) and tends to flare periodically and then subside. It may be accompanied by asthma or hay fever.
Atopic dermatitis (eczema) signs and symptoms vary widely from person to person and include:
- Itching, which may be severe, especially at night
- Red to brownish-gray patches, especially on the hands, feet, ankles, wrists, neck, upper chest, eyelids, inside the bend of the elbows and knees
- Small, raised bumps, which may leak fluid and crust over when scratched
- Thickened, cracked, dry, scaly skin
- Raw, sensitive, swollen skin from scratching
For some people, atopic dermatitis flares periodically and then clears up for a time, even for several years. Factors that can worsen atopic dermatitis signs and symptoms include:
- Dry skin, which can result from long, hot baths or showers
- Scratching, which causes further skin damage
- Bacteria and viruses
- Stress
- Sweat
- Changes in heat and humidity
- Solvents, cleaners, soaps and detergents
- Wool in clothing, blankets and carpets
- Dust and pollen
- Tobacco smoke and air pollution
- Eggs, milk, peanuts, soybeans, fish and wheat
When to see a doctor
See your doctor if:
- You're so uncomfortable that you are losing sleep or are distracted from your daily routines
- Your skin is painful
- You suspect your skin is infected (red streaks, pus, yellow scabs)
- You've tried self-care steps without success
- You think the condition is affecting your eyes or vision
Factors that put people at increased risk of developing the condition include:
- A personal or family history of eczema, allergies, hay fever or asthma
- Being a health care worker, which is linked to hand dermatitis
- Living in urban areas
- Being African-American
You're likely to start by seeing your primary care doctor. After initial evaluation, you may be referred to a specialist in skin diseases (dermatologist).
No lab test is needed to identify atopic dermatitis (eczema). Your doctor will likely make a diagnosis by examining your skin and reviewing your medical history. Atopic dermatitis can be persistent. You may need to try various treatments over months or years to control it. And even if you respond to treatment, your signs and symptoms may return (flare).
It's important to recognize the condition early so you can start treatment.
If regular moisturizing and other self-care steps don't help, your doctor may suggest the following treatments and drugs:
- Creams that control itching and inflammation. Your doctor may prescribe a corticosteroid cream or ointment.
- Drugs to fight infection. You may need antibiotics if you have a bacterial skin infection or an open sore or cracked skin caused by scratching.
- Oral anti-itch drugs. If itching is severe, oral antihistamines may help.
- Oral or injected drugs that control inflammation. For more-severe cases, your doctor may prescribe oral corticosteroids — such as prednisone — or an injected corticosteroid. These drugs are effective but can't be used long term because of potential serious side effects. Continue moisturizing and using other self-care remedies to prevent a flare-up after you stop taking the corticosteroids.
- Light therapy. The simplest form of light therapy (phototherapy) involves exposing your skin to controlled amounts of natural sunlight. Other forms use artificial ultraviolet A (UVA) and narrow band UVB either alone or with medications.
- Treatment for stress. Counseling may help people who are embarrassed or frustrated by their skin condition.
- Relaxation, behavior modification or biofeedback. These approaches may help you with habitual scratching.
Many alternative medicine therapies have helped some people manage their atopic dermatitis. One study showed that people who used Chinese herbal medications experienced reduced itching and other symptoms, but only temporarily
Evidence for the following approaches isn't conclusive:
- Dietary supplements, such as vitamins D and E, zinc, selenium, evening primrose oil, borage seed oil, oolong tea, probiotics
- Other plant-based therapies, including St. John's wort, calendula flowers, tea tree oil, German chamomile, Oregon grape root, licorice, rice bran broth (applied to the skin)
- Aromatherapy
- Bath therapy
- Use of electrodes to change electromagnetic waves of the body (bioresonance)
- Therapeutic use of color, light and relaxation techniques (chromotherapy)
- Homeopathy
- Massage therapy
The following tips may help prevent bouts of dermatitis (flares) and minimize the drying effects of bathing:
- Try to identify and avoid triggers that worsen the inflammation. Reduce your exposure to your unique triggers.
- Take shorter baths or showers. Limit your baths and showers to 10 to 15 minutes. And use warm, rather than hot, water. Bath oil also may be helpful.
- Use only gentle soaps. Choose mild soaps that clean without removing too many natural oils. Deodorant and antibacterial soaps may be more drying to your skin. Use soap only on your face, underarms, genital areas, hands and feet. Use clear water elsewhere.
- Dry yourself carefully. After bathing, brush your skin rapidly with the palms of your hands, or gently pat your skin dry with a soft towel and apply moisturizer.
- Moisturize your skin at least twice a day. Creams or lotions seal in moisture. Thicker moisturizers work best — such as Vanicream. You may also want to use cosmetics that contain moisturizers. If your skin is extremely dry, try applying baby oil or a similar product while your skin is still moist. Oil has more staying power than moisturizers do.
<Acne>
Acne is a skin condition that occurs when your hair follicles become plugged with oil and dead skin cells. Acne usually appears on your face, neck, chest, back and shoulders. Effective treatments are available, but acne can be persistent. The pimples and bumps heal slowly, and when one begins to go away, others seem to crop up.
Acne is most common among teenagers, with a reported prevalence of 70 to 87 percent. Increasingly, younger children are getting acne as well. Depending on its severity, acne can cause emotional distress and scar the skin. The earlier you start treatment, the lower your risk of lasting physical and emotional damage.
Acne signs and symptoms vary depending on the severity of your condition:
- Whiteheads (closed plugged pores)
- Blackheads (open plugged pores — the oil turns brown when it is exposed to air)
- Small red, tender bumps (papules)
- Pimples (pustules), which are papules with pus at their tips
- Large, solid, painful lumps beneath the surface of the skin (nodules)
- Painful, pus-filled lumps beneath the surface of the skin (cystic lesions)
When to see a doctor
If home care remedies don't work to clear up your acne, see your primary care doctor. He or she can prescribe stronger medications.
Four main factors cause acne:
- Oil production
- Dead skin cells
- Clogged pores
- Bacteria
Acne typically appears on your face, neck, chest, back and shoulders. These areas of skin have the most oil (sebaceous) glands. Acne occurs when hair follicles become plugged with oil and dead skin cells. Hair follicles are connected to oil glands. These glands secrete an oily substance (sebum) to lubricate your hair and skin. Sebum normally travels along the hair shafts and through the openings of the hair follicles onto the surface of your skin. When your body produces an excess amount of sebum and dead skin cells, the two can build up in the hair follicles. They form a soft plug, creating an environment where bacteria can thrive. If the clogged pore becomes infected with bacteria, inflammation results.
The plugged pore may cause the follicle wall to bulge and produce a whitehead. Or the plug may be open to the surface and may darken, causing a blackhead. A blackhead may look like dirt stuck in pores. But actually the pore is congested with bacteria and oil, which turns brown when it's exposed to the air. Pimples are raised red spots with a white center that develop when blocked hair follicles become inflamed or infected. Blockages and inflammation that develop deep inside hair follicles produce cyst-like lumps beneath the surface of your skin. Other pores in your skin, which are the openings of the sweat glands, aren't usually involved in acne.
Risk Factors for acne
- Hormones. Androgens are hormones that increase in boys and girls during puberty and cause the sebaceous glands to enlarge and make more sebum. Hormonal changes related to pregnancy and the use of oral contraceptives also can affect sebum production. And low amounts of androgens circulate in the blood of women and can worsen acne.
- Certain medications. Drugs containing corticosteroids, androgens or lithium can worsen acne.
- Diet. Studies indicate that certain dietary factors, including dairy products and carbohydrate-rich foods — such as bread, bagels and chips — may trigger acne. Chocolate has long been suspected of making acne worse. A recent study showed that eating chocolate was related to an increase in acne. Further study is needed to examine why this happens or whether acne patients need to follow specific dietary restrictions.
- Stress. Stress can make acne worse.
- Family history. Genetics plays a role in acne. If both parents had acne, you're likely to develop it, too.
- Greasy or oily substances. You may develop acne where your skin comes into contact with oily lotions and creams or with grease in a work area, such as a kitchen with fry vats.
- Friction or pressure on your skin. This can be caused by items such as telephones, cellphones, helmets, tight collars and backpacks.
If you have acne that's not responding to self-care and over-the-counter treatments, make an appointment with your primary care doctor. Early, effective treatment of acne reduces the risk of scarring and of lasting damage to your self-esteem. After an initial examination, your doctor may refer you to a specialist in the diagnosis and treatment of skin conditions (dermatologist).
Acne medications work by reducing oil production, speeding up skin cell turnover, fighting bacterial infection or reducing inflammation — which helps prevent scarring. With most prescription acne drugs, you may not see results for four to eight weeks, and your skin may get worse before it gets better. It can take many months or years for your acne to clear up completely. The drug your doctor recommends depends on the type and severity of your acne. It might be something you apply to your skin (topical medication) or take by mouth (oral medication). Often, drugs are used in combination. Pregnant women will not be able to use oral prescription medications for acne.
The most common topical prescription medications for acne are:
- Retinoids. These come as creams, gels and lotions. Retinoid drugs are derived from vitamin A and include tretinoin (Avita, Retin-A, others), adapalene (Differin) and tazarotene (Tazorac, Avage). You apply this medication in the evening, it works by preventing plugging of the hair follicles.
- Antibiotics. These work by killing excess skin bacteria and reducing redness. The antibiotics are often combined with benzoyl peroxide to reduce the likelihood of developing antibiotic resistance. Examples include clindamycin with benzoyl peroxide (Benzaclin, Duac, Acanya) and erythromycin with benzoyl peroxide (Benzamycin).
Oral medications
- Antibiotics. For moderate to severe acne, you may need oral antibiotics to reduce bacteria and fight inflammation. Choices for treating acne include tetracyclines, such as minocycline and doxycycline. You will likely use topical medications and oral antibiotics together. Studies have found that using topical benzoyl peroxide along with oral antibiotics may reduce the risk of developing antibiotic resistance.
- Combined oral contraceptives. Combined oral contraceptives are useful in treating acne in women and adolescent girls.
- Isotretinoin. This medicine is reserved for people with the most severe acne. Isotretinoin is a powerful drug for people whose acne doesn't respond to other treatments. Oral isotretinoin is very effective. But because of its potential side effects, doctors need to closely monitor anyone they treat with this drug. The most serious potential side effects include ulcerative colitis, an increased risk of depression and suicide, and severe birth defects. In fact, isotretinoin carries such serious risk of side effects that women of reproductive age must participate in a Food and Drug Administration-approved monitoring program to receive a prescription for the drug.
Therapies
- Light therapy. A variety of light-based therapies have been tried with success. But further study is needed to determine the ideal method, light source and dose. Light therapy targets the bacteria that cause acne inflammation. Some types of light therapy are done in a doctor's office. Blue-light therapy can be done at home with a hand-held device.
- Chemical peel. This procedure uses repeated applications of a chemical solution, such as salicylic acid. It is most effective when combined with other acne treatments, except oral retinoids. Chemical peels aren't recommended for people taking oral retinoids because together these treatments can significantly irritate the skin. Chemicals peels may cause temporary, severe redness, scaling and blistering, and long-term discoloration of the skin.
- Extraction of whiteheads and blackheads. Your dermatologist uses special tools to gently remove whiteheads and blackheads (comedos) that haven't cleared up with topical medications. This technique may cause scarring.
- Steroid injection. Nodular and cystic lesions can be treated by injecting a steroid drug directly into them. This improves their appearance without the need for extraction. The side effects of this technique include thinning of the skin, lighter skin and the appearance of small blood vessels on the treated area.
You can try to avoid or control mild acne with nonprescription products, good basic skin care and other self-care techniques:
- Wash problem areas with a gentle cleanser. Twice a day, use your hands to wash your face with a mild soap and warm water. If you tend to develop acne around your hairline, shampoo your hair every day. Avoid certain products, such as facial scrubs, astringents and masks, because they tend to irritate skin, which can worsen acne. Excessive washing and scrubbing also can irritate skin. And be gentle while shaving affected skin.
- Try over-the-counter acne products to dry excess oil and promote peeling. Look for products containing benzoyl peroxide as the active ingredient. You might also try products containing sulfur, resorcinol or salicylic acid. Nonprescription acne medications may cause initial side effects — such as redness, dryness and scaling — that often improve after the first month of using them.
- Avoid irritants. You may want to avoid oily or greasy cosmetics, sunscreens, hairstyling products or acne concealers. Use products labeled water-based or noncomedogenic, which means they are less likely to cause acne.
- Use an oil-free moisturizer with sunscreen. For some people, the sun worsens acne. And some acne medications make you more susceptible to the sun's rays. Check with your doctor to see if your medication is one of these. If it is, stay out of the sun as much as possible. Regularly use a nonoily (noncomedogenic) moisturizer that includes a sunscreen.
- Watch what touches your skin. Keep your hair clean and off your face. Also avoid resting your hands or objects, such as telephone receivers, on your face. Tight clothing or hats also can pose a problem, especially if you're sweating. Sweat and oils can contribute to acne.
- Don't pick or squeeze blemishes. Doing so can cause infection or scarring.
Some studies suggest that using the following supplements may help treat acne. More research is needed to establish the potential effectiveness and long-term safety of these and other natural acne treatments, traditional Chinese medicine, and ayurvedic herbs.
- Tea tree oil. Gels containing 5 percent tea tree oil may be as effective as are lotions containing 5 percent benzoyl peroxide, although tea tree oil might work more slowly. Possible side effects include contact dermatitis and, if you have rosacea, a worsening of those symptoms. One study reported that a young boy experienced breast development after using a combination lavender and tea tree oil hair product. Tea tree oil should be used only topically.
- Alpha hydroxy acid. This natural acid is found in citrus fruit and other foods. When applied to your skin, it helps remove dead skin cells and unclog pores. It may also improve the appearance of acne scars. Side effects include increased sensitivity to the sun, redness, mild stinging and skin irritation.
- Azelaic acid. This natural acid is found in whole-grain cereals and animal products. It has antibacterial properties. A 20 percent azelaic acid cream seems to be as effective as many other conventional acne treatments when used twice a day for at least four weeks. It is even more effective when used in combination with erythromycin. Prescription azelaic acid (Azelex, Finacea) is an option during pregnancy and while breastfeeding.
- Bovine cartilage. Creams containing 5 percent bovine cartilage, applied to the affected skin twice a day, may be effective in reducing acne.
- Zinc. Zinc in lotions and creams may reduce acne breakouts.
- Green tea extract. A lotion of 2 percent green tea extract helped reduce acne in two studies of adolescents and young adults with mild to moderate acne.
- Aloe vera. A 50 percent aloe vera gel was combined with a conventional acne drug (tretinoin) and tested for 8 weeks on 60 people with moderate acne. The combination approach was significantly more effective than tretinoin alone.
- Probiotics. Certain probiotic strains seems to help decrease acne.
<Rosacea>
Rosacea is a common skin condition that causes redness in your face and often produces small, red, pus-filled bumps. Although rosacea can occur in anyone, it most commonly affects middle-aged women who have fair skin. Left untreated, rosacea tends to worsen over time. Rosacea signs and symptoms may flare up for a period of weeks to months and then diminish before flaring up again. Rosacea can be mistaken for acne, an allergic reaction or other skin problems.
Signs and symptoms of rosacea may include:
- Facial redness. Rosacea usually causes a persistent redness in the central portion of your face. Small blood vessels on your nose and cheeks often swell and become visible.
- Swollen red bumps. Many people who have rosacea also develop bumps on their face that resemble acne. These bumps sometimes contain pus. Your skin may feel hot and tender.
- Eye problems. About half of the people who have rosacea also experience eye dryness, irritation and swollen, reddened eyelids. In some people, rosacea's eye symptoms precede the skin symptoms.
- Enlarged nose. Rarely, rosacea can thicken the skin on the nose, causing the nose to appear bulbous (rhinophyma). This occurs more often in men than in women.
When to see a doctor
If you experience persistent redness of your face, see your primary care doctor for a diagnosis and proper treatment.
A number of factors can trigger or aggravate rosacea by increasing blood flow to the surface of your skin. Some of these factors include:
- Hot foods or beverages
- Spicy foods
- Alcohol
- Temperature extremes
- Sunlight
- Stress, anger or embarrassment
- Strenuous exercise
- Hot baths or saunas
- Corticosteroids, such as prednisone
Although anyone can develop rosacea, you may be more likely to develop rosacea if you:
- Are a woman
- Have fair skin
- Are between the ages of 30 and 60
- Have a family history of rosacea
In severe and rare cases, the oil glands (sebaceous glands) in your nose and sometimes your cheeks become enlarged, resulting in a buildup of tissue on and around your nose — a condition called rhinophyma. This complication is much more common in men and develops slowly over a period of years.
Medications
- Antibiotics. The antibiotics used for rosacea also have anti-inflammation effects. They may come in the form of creams, gels or lotions to spread on the affected skin or in pills that you swallow. Antibiotic pills are generally more effective in the short term, but they can also cause more side effects.
- Acne drugs. If antibiotics don't work, your doctor might suggest trying isotretinoin (Amnesteem, Claravis, others). This powerful drug is most commonly used for severe cystic acne, but it also often helps clear up acne-like lesions of rosacea. Don't use this drug during pregnancy as it can cause serious birth defects.
The duration of your treatment depends on the type and severity of your symptoms, but typically you'll notice an improvement within one to two months. Because symptoms may recur if you stop taking medications, long-term regular treatment is often necessary.
Enlarged blood vessels, some redness and changes due to rhinophyma often become permanent. In these cases, surgical methods, such as laser surgery and electrosurgery, may reduce the visibility of blood vessels, remove tissue buildup around your nose and generally improve your appearance.
One of the most important things you can do if you have rosacea is to minimize your exposure to anything that causes a flare-up. Find out what factors affect you so that you can avoid them. Other suggestions to prevent flare-ups include:
- Wear broad-spectrum sunscreen with an SPF of 30 or higher
- Protect your face in the winter with a scarf or ski mask
- Avoid irritating your facial skin by rubbing or touching it too much
- Wash problem areas with a gentle cleanser (Dove, Cetaphil)
- Avoid facial products that contain alcohol or other skin irritants
If you wear makeup, consider using green-tinted foundation creams and powders because they're designed to counter skin redness.
Many alternative therapies — including colloidal silver, emu oil, laurelwood, oregano oil and vitamin K — have been touted as possible ways to treat rosacea. However, there's no conclusive evidence that any of these alternative therapies are effective.
<Ringworm>
Ringworm of the body is a fungal infection that develops on the top layer of your skin. It's characterized by a red circular rash with clearer skin in the middle. It may or may not itch. Ringworm gets its name because of its appearance. There is no actual worm involved. Also called tinea corporis, ringworm of the body is closely related to athlete's foot (tinea pedis), jock itch (tinea cruris) and ringworm of the scalp (tinea capitis). Ringworm often spreads by direct skin-to-skin contact with an infected person or animal.
Antifungal medications are used to treat ringworm. Mild ringworm often responds to antifungal products that you apply to your skin. For more-severe infections, you may need to take antifungal pills for several weeks.
Ringworm typically begins as a flat scaly area on the skin, which may be red and itchy. This patch develops a slightly raised border that expands outward — forming a roughly circular ring. The contours of the ring may be quite irregular, resembling the wavy outline of a snake or a worm. The interior of the ring may be clear, scaly or marked with a scattering of red bumps. In some people, several rings develop at the same time and may overlap.
When to see a doctor
See your primary care doctor if you have a rash on your skin that doesn't begin to improve within two weeks. You may need prescription medication.
Ringworm is a contagious fungal infection caused by mold-like parasites that live on the cells in the outer layer of your skin. It can be spread in the following ways:
- Human to human. Ringworm often spreads by direct, skin-to-skin contact with an infected person.
- Animal to human. You can contract ringworm by touching an animal with ringworm. Ringworm can spread while petting or grooming dogs or cats. It's also fairly common in cows.
- Object to human. Ringworm can spread by contact with objects or surfaces that an infected person or animal has recently touched or rubbed against, such as clothing, towels, bedding and linens, combs, and brushes.
- Soil to human. In rare cases, ringworm can be spread to humans by contact with infected soil. Infection would most likely occur only from prolonged contact with highly infected soil.
You're at higher risk of ringworm of the body if you:
- Are a child younger than 15 years old
- Live in damp, humid or crowded conditions
- Have close contact with an infected person or animal
- Share clothing, bedding or towels with someone who has a fungal infection
- Participate in sports that feature skin-to-skin contact, such as wrestling
- Wear tight or restricted clothing
- Have a weakened immune system
A fungal infection rarely spreads below the surface of the skin to cause serious illness. However, people with weak immune systems, such as those with HIV/AIDS, may find it difficult to get rid of the infection.
Ringworm is difficult to prevent. The fungus that causes ringworm is common and contagious even before symptoms appear. However, you can help reduce your risk of ringworm by taking these steps:
- Educate yourself and others. Be aware of the risk of ringworm from infected people or pets. Tell your children about ringworm, what to watch for and how to avoid the infection.
- Keep clean. Wash your hands often to avoid the spread of infection. Keep common or shared areas clean, especially in schools, child care centers, gyms and locker rooms.
- Stay cool and dry. Don't wear thick clothing for long periods of time in warm, humid weather. Avoid excessive sweating.
- Avoid infected animals. The infection often looks like a patch of skin where fur is missing. In some cases, though, you may not notice any signs of the disease. Ask your veterinarian to check your pets and domesticated animals for ringworm.
- Don't share personal items. Don't let others use your clothing, towels, hairbrushes or other personal items. Refrain from borrowing these items from others as well.
<Psoriasis>
Psoriasis is a common skin condition that changes the life cycle of skin cells. Psoriasis causes cells to build up rapidly on the surface of the skin. The extra skin cells form thick, silvery scales and itchy, dry, red patches that are sometimes painful. Psoriasis is a persistent, long-lasting (chronic) disease. There may be times when your psoriasis symptoms get better alternating with times your psoriasis worsens.
The primary goal of treatment is to stop the skin cells from growing so quickly. While there isn't a cure, psoriasis treatments may offer significant relief. Lifestyle measures, such as using a nonprescription cortisone cream and exposing your skin to small amounts of natural sunlight, also may improve your psoriasis symptoms.
Psoriasis signs and symptoms can vary from person to person but may include one or more of the following:
- Red patches of skin covered with silvery scales
- Small scaling spots
- Dry, cracked skin that may bleed
- Itching, burning or soreness
- Thickened, pitted or ridged nails
- Swollen and stiff joints
When to see a doctor
See your primary care doctor If you suspect that you may have psoriasis, and if your signs and symptoms worsen or don't improve with self care.
The cause of psoriasis isn't fully known, but it's thought to be related to an immune system problem with cells in your body. More specifically, one key cell is a type of white blood cell called a T lymphocyte or T cell. Normally, T cells travel throughout the body to detect and fight off foreign substances, such as viruses or bacteria. If you have psoriasis, however, the T cells attack healthy skin cells by mistake, as if to heal a wound or to fight an infection. Overactive T cells trigger other immune responses. The effects include dilation of blood vessels in the skin around the plaques and an increase in other white blood cells that can enter the outer layer of skin. These changes result in an increased production of both healthy skin cells and more T cells and other white blood cells. This causes an ongoing cycle in which new skin cells move to the outermost layer of skin too quickly — in days rather than weeks. Dead skin and white blood cells can't slough off quickly enough and build up in thick, scaly patches on the skin's surface. This usually doesn't stop unless treatment interrupts the cycle.
Factors that may trigger psoriasis include:
- Infections, such as strep throat or skin infections
- Injury to the skin, such as a cut or scrape, bug bite, or a severe sunburn
- Stress
- Cold weather
- Smoking
- Heavy alcohol consumption
- Certain medications — including lithium, which is prescribed for bipolar disorder; antimalarial drugs; and iodides.
Anyone can develop psoriasis, but these factors can increase your risk of developing the disease:
- Family history. Perhaps the most significant risk factor for psoriasis is having a family history of the disease. Having one parent with psoriasis increases your risk of getting the disease, and having two parents with psoriasis increases your risk even more.
- Viral and bacterial infections. People with HIV are more likely to develop psoriasis than people with healthy immune systems are. Children and young adults with recurring infections, particularly strep throat, also may be at increased risk.
- Stress. Because stress can impact your immune system, high stress levels may increase your risk of psoriasis.
- Obesity. Excess weight increases the risk of psoriasis. Plaques associated with all types of psoriasis often develop in skin creases and folds.
- Smoking. Smoking tobacco not only increases your risk of psoriasis but also may increase the severity of the disease. Smoking may also play a role in the initial development of the disease.
If you have psoriasis, you're at greater risk of developing certain diseases.
- Psoriatic arthritis. This complication of psoriasis can cause joint damage and a loss of function in some joints, which can be debilitating.
- Eye conditions. Certain eye disorders — such as conjunctivitis, blepharitis and uveitis — are more common in people with psoriasis.
- Type 2 diabetes. The risk of type 2 diabetes is increased in people with psoriasis. The more severe the psoriasis, the greater the likelihood of type 2 diabetes.
- High blood pressure. The odds of having high blood pressure are higher for people with psoriasis.
- Cardiovascular disease. For people with psoriasis, the risk of heart attack is almost three times greater than for those without the disease. The risk of irregular heartbeats and stroke is also higher in those with psoriasis
- Metabolic syndrome. This is a cluster of conditions — including high blood pressure, elevated insulin levels and abnormal cholesterol levels — that increases your risk of heart disease. People with psoriasis have a higher risk of metabolic syndrome.
- Other autoimmune diseases. Celiac disease, sclerosis and the inflammatory bowel disease called Crohn's disease are more likely to strike people with psoriasis.
- Parkinson's disease. This chronic neurological condition is more likely to occur in people with psoriasis.
- Kidney disease. Moderate to severe psoriasis has been linked to a higher risk of kidney disease.
Psoriasis can also affect your quality of life by increasing your risk of:
- Low self-esteem
- Depression
- Social isolation
- Problems at work, which can lead to a lower income
You'll likely first see your primary care doctor. In some cases, you may be referred to a specialist in skin diseases (dermatologist). In most cases, diagnosis of psoriasis is fairly straightforward.
- Physical exam and medical history. Your doctor usually can diagnose psoriasis by taking your medical history and examining your skin, scalp and nails.
- Skin biopsy. Rarely, your doctor may take a small sample of skin (biopsy) that's examined under a microscope to determine the exact type of psoriasis and to rule out other disorders. A skin biopsy can generally be done in a dermatologist's office after application of a local anesthetic.
Psoriasis treatments can be divided into three main types: topical treatments, light therapy and systemic medications.
Topical treatments
- Topical corticosteroids. These powerful anti-inflammatory drugs are the most frequently prescribed medications for treating mild to moderate psoriasis. They slow cell turnover by suppressing the immune system, which reduces inflammation and relieves associated itching. Topical corticosteroids range in strength, from mild to very strong.
Low-potency corticosteroid ointments are usually recommended for sensitive areas, such as your face or skin folds, and for treating widespread patches of damaged skin. Your doctor may prescribe stronger corticosteroid ointment for small areas of your skin, for persistent plaques on your hands or feet, or when other treatments have failed. - Vitamin D analogues. These synthetic forms of vitamin D slow down the growth of skin cells. Calcipotriene (Dovonex) is a prescription cream or solution containing a vitamin D analogue that may be used alone to treat mild to moderate psoriasis or in combination with other topical medications or phototherapy.
- Anthralin. This medication is believed to normalize DNA activity in skin cells. Anthralin (Dritho-Scalp) also can remove scale, making the skin smoother. However, anthralin can irritate skin, and it stains virtually anything it touches, including skin, clothing, countertops and bedding. For that reason, doctors often recommend short-contact treatment — allowing the cream to stay on your skin for a brief time before washing it off.
- Topical retinoids. These are commonly used to treat acne and sun-damaged skin, but tazarotene (Tazorac, Avage) was developed specifically for the treatment of psoriasis. Like other vitamin A derivatives, it normalizes DNA activity in skin cells and may decrease inflammation. The most common side effect is skin irritation. It may also increase sensitivity to sunlight, so sunscreen should be applied while using the medication. Although the risk of birth defects is far lower for topical retinoids than for oral retinoids, tazarotene isn't recommended when you're pregnant or breast-feeding or if you intend to become pregnant.
- Salicylic acid. Available over-the-counter (nonprescription) and by prescription, salicylic acid promotes sloughing of dead skin cells and reduces scaling. Sometimes it's combined with other medications, such as topical corticosteroids or coal tar, to increase its effectiveness. Salicylic acid is available in medicated shampoos and scalp solutions to treat scalp psoriasis.
- Moisturizers. By themselves, moisturizing creams won't heal psoriasis, but they can reduce itching and scaling and can help combat the dryness that results from other therapies. Moisturizers in an ointment base are usually more effective than are lighter creams and lotions.
Light therapy
- Sunlight. Ultraviolet (UV) light is a wavelength of light in a range too short for the human eye to see. When exposed to UV rays in sunlight or artificial light, the activated T cells in the skin die. This slows skin cell turnover and reduces scaling and inflammation. Brief, daily exposures to small amounts of sunlight may improve psoriasis, but intense sun exposure can worsen symptoms and cause skin damage.
- UVB phototherapy. Controlled doses of UVB light from an artificial light source may improve mild to moderate psoriasis symptoms.
- Photochemotherapy or psoralen plus ultraviolet A (PUVA). Photochemotherapy involves taking a light-sensitizing medication (psoralen) before exposure to UVA light. UVA light penetrates deeper into the skin than does UVB light, and psoralen makes the skin more responsive to UVA exposure. This more aggressive treatment consistently improves skin and is often used for more-severe cases of psoriasis. PUVA involves two or three treatments a week for a prescribed number of weeks. Because this treatment makes you more sensitive to sunlight, it's important to avoid sun exposure when possible and to wear a broad-spectrum sunscreen with an SPF of at least 30. To protect your eyes, wear UVA-protective sunglasses.
- Excimer laser. This form of light therapy, used for mild to moderate psoriasis, treats only the involved skin. A controlled beam of UVB light of a specific wavelength is directed to the psoriasis plaques to control scaling and inflammation. Healthy skin surrounding the patches isn't harmed. Excimer laser therapy requires fewer sessions than does traditional phototherapy because more powerful UVB light is used.
Oral or injected medication
- Retinoids. Related to vitamin A, this group of drugs may reduce the production of skin cells if you have severe psoriasis that doesn't respond to other therapies.
- Methotrexate. Taken orally, methotrexate helps psoriasis by decreasing the production of skin cells and suppressing inflammation. It may also slow the progression of psoriatic arthritis in some people.
- Cyclosporine. Cyclosporine suppresses the immune system and is similar to methotrexate in effectiveness.
- Drugs that alter the immune system (biologics). Several immunomodulator drugs are approved for the treatment of moderate to severe psoriasis. They include etanercept (Enbrel), infliximab (Remicade), adalimumab (Humira) and ustekinumab (Stelara). These drugs are given by intravenous infusion, intramuscular injection or subcutaneous injection and are usually used for people who have failed to respond to traditional therapy or who have associated psoriatic arthritis. Biologics work by blocking interactions between certain immune system cells and particular inflammatory pathways. Although they're derived from natural sources rather than chemical ones, they must be used with caution because they have strong effects on the immune system and may permit life-threatening infections. In particular, people taking these treatments must be screened for tuberculosis.
Although doctors choose treatments based on the type and severity of psoriasis and the areas of skin affected, the traditional approach is to start with the mildest treatments — topical creams and ultraviolet light therapy (phototherapy) — and then progress to stronger ones only if necessary. The goal is to find the most effective way to slow cell turnover with the fewest possible side effects. In spite of a range of options, effective treatment of psoriasis can be challenging. The disease is unpredictable, going through cycles of improvement and worsening, seemingly at random. Effects of psoriasis treatments also can be unpredictable; what works well for one person might be ineffective for someone else.
Although self-help measures won't cure psoriasis, they may help improve the appearance and feel of damaged skin.
- Take daily baths. Bathing daily helps remove scales and calm inflamed skin. Add bath oil, colloidal oatmeal, Epsom salts or Dead Sea salts to the water and soak. Avoid hot water and harsh soaps, which can worsen symptoms; use lukewarm water and mild soaps that have added oils and fats.
- Use moisturizer. Blot your skin after bathing, then immediately apply a heavy, ointment-based moisturizer while your skin is still moist. For very dry skin, oils may be preferable — they have more staying power than creams or lotions do and are more effective at preventing water from evaporating from your skin. During cold, dry weather, you may need to apply a moisturizer several times a day.
- Expose your skin to small amounts of sunlight. A controlled amount of sunlight can significantly improve lesions, but too much sun can trigger or worsen outbreaks and increase the risk of skin cancer. Keep a record of when and how long you're in the sun to help avoid overexposure. And be sure to protect healthy, unaffected skin with a broad-spectrum sunscreen with an SPF of at least 30. Apply sunscreen generously, and reapply every two hours — or more often if you're swimming or perspiring.
- Avoid psoriasis triggers, if possible. Find out what triggers, if any, worsen your psoriasis and take steps to prevent or avoid them. Infections, injuries to your skin, stress, smoking and intense sun exposure can all worsen psoriasis.
- Avoid drinking alcohol. Alcohol consumption may decrease the effectiveness of some psoriasis treatments.
A number of alternative therapies claim to ease the symptoms of psoriasis, including special diets, creams, dietary supplements and herbs. None have definitively been proved effective. But some alternative therapies are deemed generally safe, and they may be helpful to some people in reducing signs and symptoms, such as itching and scaling.
- Aloe vera. Taken from the leaves of the aloe vera plant, aloe extract cream may reduce redness, scaling, itching and inflammation. You may need to use the cream several times a day for a month or more to see any improvements in your skin.
- Fish oil. Omega-3 fatty acids found in fish oil supplements may reduce inflammation associated with psoriasis, although results from studies are mixed. Taking 3 grams or less of fish oil daily is generally recognized as safe, and you may find it beneficial.
- Oregon grape. Also known as barberry, topical applications of Oregon grape may reduce inflammation and ease psoriasis symptoms.
<Shingles>
Shingles is a viral infection that causes a painful rash. Although shingles can occur anywhere on your body, it most often appears as a single stripe of blisters that wraps around either the left or the right side of your torso. Shingles is caused by the varicella-zoster virus — the same virus that causes chickenpox. After you've had chickenpox, the virus lies inactive in nerve tissue near your spinal cord and brain. Years later, the virus may reactivate as shingles.
While it isn't a life-threatening condition, shingles can be very painful. Vaccines can help reduce the risk of shingles, while early treatment can help shorten a shingles infection and lessen the chance of complications.
The signs and symptoms of shingles may include:
- Pain, burning, numbness or tingling
- Sensitivity to touch
- A red rash that begins a few days after the pain
- Fluid-filled blisters that break open and crust over
- Itching
- Fever
- Headache
- Sensitivity to light
- Fatigue
Pain is usually the first symptom of shingles. For some, it can be intense. Depending on the location of the pain, it can sometimes be mistaken for a symptom of problems affecting the heart, lungs or kidneys. Some people experience shingles pain without ever developing the rash.
When to see a doctor
Contact your primary care doctor promptly if you suspect shingles, but especially in the following situations:
- The pain and rash occur near an eye. If left untreated, this infection can lead to permanent eye damage.
- You're 70 or older, because age significantly increases your risk of complications.
- You or someone in your family has a weakened immune system (due to cancer, medications or chronic illness).
- The rash is widespread and painful.
Are you contagious?A person with shingles can pass the varicella-zoster virus to anyone who isn't immune to chickenpox. This usually occurs through direct contact with the open sores of the shingles rash. Once infected, the person will develop chickenpox, however, not shingles.
Chickenpox can be dangerous for some groups of people. Until your shingles blisters scab over, you are contagious and should avoid physical contact with:
- Anyone who has a weak immune system
- Newborns
- Pregnant women
Anyone who has ever had chickenpox can develop shingles. Most adults in the United States had chickenpox when they were children, before the advent of the routine childhood vaccination that now protects against chickenpox.
Factors that may increase your risk of developing shingles include:
- Being older than 50. Shingles is most common in people older than 50. The risk increases with age. Some experts estimate that half the people 80 and older will have shingles.
- Having certain diseases. Diseases that weaken your immune system, such as HIV/AIDS and cancer, can increase your risk of shingles.
- Undergoing cancer treatments. Radiation or chemotherapy can lower your resistance to diseases and may trigger shingles.
- Taking certain medications. Drugs designed to prevent rejection of transplanted organs can increase your risk of shingles — as can prolonged use of steroids, such as prednisone.
Shingles is usually diagnosed based on the history of pain on one side of your body, along with the telltale rash and blisters. There's no cure for shingles, but prompt treatment with prescription antiviral drugs can speed healing and reduce your risk of complications.
These medications include:
- Acyclovir (Zovirax)
- Valacyclovir (Valtrex)
- Famciclovir (Famvir)
Shingles can cause severe pain, so your doctor also may prescribe:
- Anticonvulsants, such as gabapentin (Neurontin)
- Tricyclic antidepressants, such as amitriptyline
- Medications that contain narcotics, such as codeine
- Corticosteroids
Shingles generally lasts between two and six weeks. Most people get shingles only once, but it is possible to get it two or more times. Taking a cool bath or using cool, wet compresses on your blisters may help relieve the itching and pain. And, if possible, try to reduce the amount of stress in your life.
Two vaccines may help prevent shingles — the chickenpox (varicella) vaccine and the shingles (varicella-zoster) vaccine. Chickenpox vaccine has become a routine childhood immunization to prevent chickenpox. The vaccine is also recommended for adults who've never had chickenpox. Though the vaccine doesn't guarantee you won't get chickenpox or shingles, it can reduce your chances of complications and reduce the severity of the disease. The Food and Drug Administration has approved the use of the varicella-zoster vaccine (Zostavax) for adults age 50 and older. Like the chickenpox vaccine, the shingles vaccine doesn't guarantee you won't get shingles. But this vaccine will likely reduce the course and severity of the disease and reduce your risk of postherpetic neuralgia. The shingles vaccine is used only as a prevention strategy, however. It's not intended to treat people who currently have the disease. The vaccine contains live virus and should not be given to people who have weakened immune systems.
<Moles>
Moles are a common type of growth on the skin. They often appear as small, dark brown spots and are caused by clusters of pigmented cells. Moles generally appear during childhood and adolescence. Most people have 10 to 45 moles, almost all of which appear before age 40. Some moles may fade or disappear as you age.
Most moles are harmless. Rarely, they become cancerous. Monitoring moles and other pigmented patches is an important step in detecting skin cancer, especially malignant melanoma. Unusual moles that may indicate melanoma. This ABCDE guide can help you determine if a mole or a spot may be melanoma:
- A is for asymmetrical shape. One half is unlike the other half.
- B is for border. Look for moles with irregular, notched or scalloped borders.
- C is for color. Look for growths that have changed color, have many colors or have uneven color.
- D is for diameter. Look for new growth in a mole larger than 1/4 inch (about 6 millimeters).
- E is for evolving. Watch for moles that change in size, shape, color or height, especially if part or all of a mole turns black.
Cancerous (malignant) moles vary greatly in appearance. Some may show all of the features listed above. Others may have only one or two.
When to see a doctor
See your doctor if you have a mole that:
- Is painful
- Itches or burns
- Oozes or bleeds
- Shows any of the ABCDE characteristics listed above
- Grows back after having been removed before
- Is new and you're over 30 years old
Melanoma is the main complication of moles. Some people have a higher than average risk of their moles becoming cancerous and developing into melanoma. Factors that increase your risk of melanoma include:
- Being born with large moles. These types of moles are called congenital nevi. On an infant, such moles are classified as large if they're more than 2 inches (5 centimeters) in diameter.
- Having unusual moles. Moles that are bigger than a common mole and irregular in shape are known as atypical (dysplastic) nevi. They tend to be hereditary. And they often have dark brown centers and lighter, uneven borders.
- Having many moles. Having more than 50 ordinary moles on your body indicates an increased risk of melanoma. Two recent studies add to the evidence that the number of your moles predict cancer risk. One showed that people with 20 or more moles on their arms are at increased risk of melanoma. Another showed a relationship between the number of women's moles and breast cancer risk.
- Having a family history of melanoma. Some types of atypical moles lead to a genetic form of melanoma.
If your doctor suspects that a mole may be cancerous, he or she may take a tissue sample (biopsy) and submit it for microscopic examination. If your mole is cancerous, your doctor will do a surgical procedure to remove it. If you have a mole in the beard area, you may want to have it removed by your doctor because shaving over it repeatedly may cause irritation. You may also want to have moles removed from other parts of your body that are vulnerable to trauma and friction.
Mole removal takes only a short time and is usually done on an outpatient basis. The procedure may leave a permanent scar. If you notice that a mole has grown back, see your doctor promptly.
Take measures to protect your skin from ultraviolet (UV) radiation, such as from the sun or tanning beds. UV radiation has been linked to increased melanoma risk. And children who haven't been protected from sun exposure tend to develop more moles.
- Avoid peak sun times. It's best to avoid overexposure to the sun. If you must be outdoors, try to stay out of the sun from 10 a.m. to 4 p.m., when UV rays are strongest.
- Use sunscreen year-round. Apply sunscreen about 30 minutes before going outdoors, even on cloudy days. Use a broad-spectrum sunscreen with an SPF of at least 15. Apply it generously and reapply every two hours — or more often if you're swimming or sweating. The American Academy of Dermatology recommends using a broad-spectrum, water-resistant sunscreen with an SPF of at least 30.
- Cover up. Sunglasses, broad-brimmed hats, long sleeves and other protective clothing can help you avoid damaging UV rays. You might also want to consider clothing that's made with fabric specially treated to block UV radiation.
- Avoid tanning beds. Tanning beds emit UV rays and can increase your risk of skin cancer.
<Skin cancer>
Skin cancer — the abnormal growth of skin cells — most often develops on skin exposed to the sun. But this common form of cancer can also occur on areas of your skin not ordinarily exposed to sunlight.
There are three major types of skin cancer — basal cell carcinoma, squamous cell carcinoma and melanoma.
You can reduce your risk of skin cancer by limiting or avoiding exposure to ultraviolet (UV) radiation. Checking your skin for suspicious changes can help detect skin cancer at its earliest stages. Early detection of skin cancer gives you the greatest chance for successful skin cancer treatment. Skin cancer affects people of all skin tones, including those with darker complexions. When melanoma occurs in people with dark skin tones, it's more likely to occur in areas not normally exposed to the sun.
Basal cell carcinoma may appear as:
- A pearly or waxy bump
- A flat, flesh-colored or brown scar-like lesion
Squamous cell carcinoma may appear as:
- A firm, red nodule
- A flat lesion with a scaly, crusted surface
Melanoma signs include:
- A large brownish spot with darker speckles
- A mole that changes in color, size or feel or that bleeds
- A small lesion with an irregular border and portions that appear red, white, blue or blue-black
- Dark lesions on your palms, soles, fingertips or toes, or on mucous membranes lining your mouth, nose, vagina or anus
When to see a doctor
Make an appointment with your primary care doctor if you notice any changes to your skin that worry you.
Skin cancer occurs when errors (mutations) occur in the DNA of skin cells. The mutations cause the cells to grow out of control and form a mass of cancer cells. Much of the damage to DNA in skin cells results from ultraviolet (UV) radiation found in sunlight and in the lights used in tanning beds. But sun exposure doesn't explain skin cancers that develop on skin not ordinarily exposed to sunlight. This indicates that other factors may contribute to your risk of skin cancer, such as being exposed to toxic substances or having a condition that weakens your immune system.
Factors that may increase your risk of skin cancer include:
- Fair skin. Anyone, regardless of skin color, can get skin cancer. However, having less pigment (melanin) in your skin provides less protection from damaging UV radiation. If you have blond or red hair and light-colored eyes, and you freckle or sunburn easily, you're much more likely to develop skin cancer than is a person with darker skin.
- A history of sunburns. Having had one or more blistering sunburns as a child or teenager increases your risk of developing skin cancer as an adult. Sunburns in adulthood also are a risk factor.
- Excessive sun exposure. Anyone who spends considerable time in the sun may develop skin cancer, especially if the skin isn't protected by sunscreen or clothing. Tanning, including exposure to tanning lamps and beds, also puts you at risk. A tan is your skin's injury response to excessive UV radiation.
- Sunny or high-altitude climates. People who live in sunny, warm climates are exposed to more sunlight than are people who live in colder climates. Living at higher elevations, where the sunlight is strongest, also exposes you to more radiation.
- Moles. People who have many moles or abnormal moles called dysplastic nevi are at increased risk of skin cancer. These abnormal moles — which look irregular and are generally larger than normal moles — are more likely than others to become cancerous. If you have a history of abnormal moles, watch them regularly for changes.
- Precancerous skin lesions. Having skin lesions known as actinic keratosis can increase your risk of developing skin cancer. These precancerous skin growths typically appear as rough, scaly patches that range in color from brown to dark pink. They're most common on the face, head and hands of fair-skinned people whose skin has been sun damaged.
- A family history of skin cancer. If one of your parents or a sibling has had skin cancer, you may have an increased risk of the disease.
- A personal history of skin cancer. If you developed skin cancer once, you're at risk of developing it again.
- A weakened immune system. People with weakened immune systems have a greater risk of developing skin cancer. This includes people living with HIV/AIDS and those taking immunosuppressant drugs after an organ transplant.
- Exposure to radiation. People who received radiation treatment for skin conditions such as eczema and acne may have an increased risk of skin cancer, particularly basal cell carcinoma.
- Exposure to certain substances. Exposure to certain substances, such as arsenic, may increase your risk of skin cancer.
Your treatment options for skin cancer and the precancerous skin lesions known as actinic keratoses will vary, depending on the size, type, depth and location of the lesions. Small skin cancers limited to the surface of the skin may not require treatment beyond an initial skin biopsy that removes the entire growth.
If additional treatment is needed, options may include:
- Freezing. Your doctor may destroy actinic keratoses and some small, early skin cancers by freezing them with liquid nitrogen (cryosurgery). The dead tissue sloughs off when it thaws.
- Excisional surgery. This type of treatment may be appropriate for any type of skin cancer. Your doctor cuts out (excises) the cancerous tissue and a surrounding margin of healthy skin. A wide excision — removing extra normal skin around the tumor — may be recommended in some cases.
- Mohs surgery. This procedure is for larger, recurring or difficult-to-treat skin cancers, which may include both basal and squamous cell carcinomas. It's often used in areas where it's necessary to conserve as much skin as possible, such as on the nose. During Mohs surgery, your doctor removes the skin growth layer by layer, examining each layer under the microscope, until no abnormal cells remain. This procedure allows cancerous cells to be removed without taking an excessive amount of surrounding healthy skin.
- Curettage and electrodesiccation or cryotherapy. After removing most of a growth, your doctor scrapes away layers of cancer cells using a device with a circular blade (curet). An electric needle destroys any remaining cancer cells. In a variation of this procedure, liquid nitrogen can be used to freeze the base and edges of the treated area.
Radiation therapy. Radiation therapy uses high-powered energy beams, such as X-rays, to kill cancer cells. Radiation therapy may be an option when cancer can't be completely removed during surgery. - Chemotherapy.In chemotherapy, drugs are used to kill cancer cells. For cancers limited to the top layer of skin, creams or lotions containing anti-cancer agents may be applied directly to the skin. Systemic chemotherapy can be used to treat skin cancers that have spread to other parts of the body.
- Photodynamic therapy. This treatment destroys skin cancer cells with a combination of laser light and drugs that makes cancer cells sensitive to light.
- Biological therapy. Biological treatments stimulate your immune system in order to kill cancer cells.
Most skin cancers are preventable. To protect yourself, follow these skin cancer prevention tips:
- Avoid the sun during the middle of the day. For many people in North America, the sun's rays are strongest between about 10 a.m. and 4 p.m. Schedule outdoor activities for other times of the day, even in winter or when the sky is cloudy. You absorb UV radiation year-round, and clouds offer little protection from damaging rays. Avoiding the sun at its strongest helps you avoid the sunburns and suntans that cause skin damage and increase your risk of developing skin cancer. Sun exposure accumulated over time also may cause skin cancer.
- Wear sunscreen year-round. Sunscreens don't filter out all harmful UV radiation, especially the radiation that can lead to melanoma. But they play a major role in an overall sun protection program. Use a broad-spectrum sunscreen with an SPF of at least 15. Apply sunscreen generously, and reapply every two hours — or more often if you're swimming or perspiring. Use a generous amount of sunscreen on all exposed skin, including your lips, the tips of your ears, and the backs of your hands and neck.
- Wear protective clothing. Sunscreens don't provide complete protection from UV rays. So cover your skin with dark, tightly woven clothing that covers your arms and legs, and a broad-brimmed hat, which provides more protection than a baseball cap or visor does. Don't forget sunglasses. Look for those that block both types of UV radiation — UVA and UVB rays.
- Avoid tanning beds. Lights used in tanning beds emit UV rays and can increase your risk of skin cancer.
- Check your skin regularly and report changes to your doctor. Examine your skin often for new skin growths or changes in existing moles, freckles, bumps and birthmarks.