Lung cancer is a type of cancer that begins in the lungs. Your lungs are two spongy organs in your chest that take in oxygen when you inhale and release carbon dioxide when you exhale.
Lung cancer is the leading cause of cancer deaths in the United States, among both men and women. Lung cancer claims more lives each year than do colon, prostate, ovarian and breast cancers combined.
People who smoke have the greatest risk of lung cancer. The risk of lung cancer increases with the length of time and number of cigarettes you've smoked. If you quit smoking, even after smoking for many years, you can significantly reduce your chances of developing lung cancer.
Lung cancer typically doesn't cause signs and symptoms in its earliest stages. Signs and symptoms of lung cancer typically occur only when the disease is advanced.
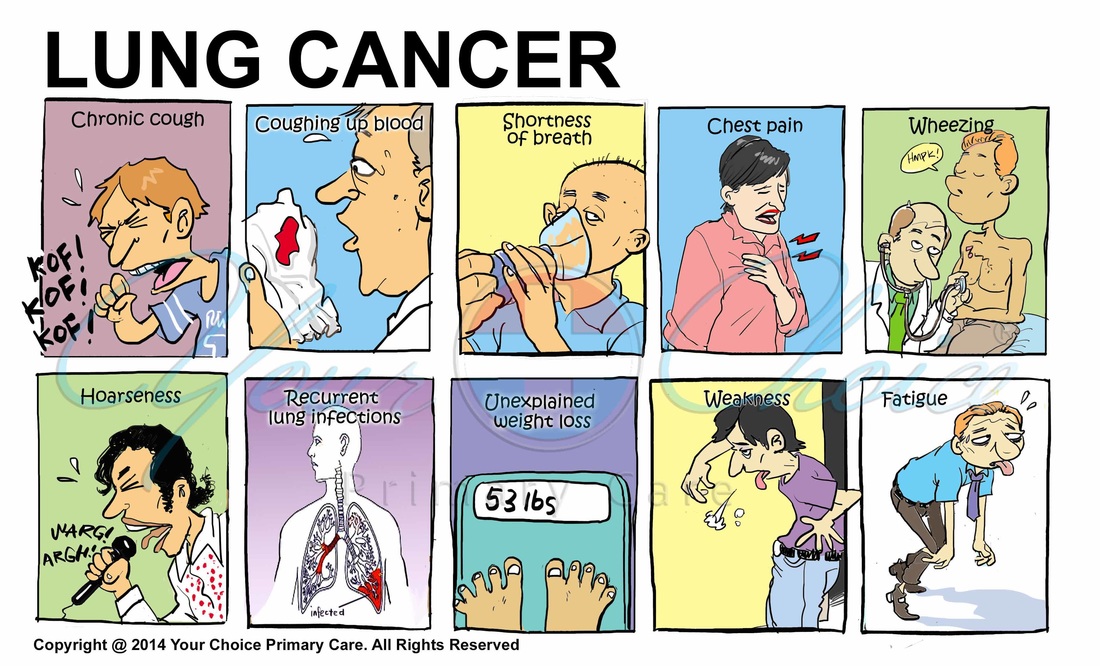
Signs and symptoms of lung cancer may include:
- A new cough that doesn't go away
- Changes in a chronic cough or "smoker's cough"
- Coughing up blood, even a small amount
- Shortness of breath
- Chest pain
- Wheezing
- Hoarseness
- Losing weight without trying
- Bone pain
- Headache
When to see a doctor
Make an appointment with your primary care doctor if you have any signs or symptoms that worry you.
If you smoke and have been unable to quit, make an appointment with your doctor. Your doctor can recommend strategies for quitting smoking, such as counseling, medications and nicotine replacement products.
Smoking causes the majority of lung cancers — both in smokers and in people exposed to secondhand smoke. But lung cancer also occurs in people who never smoked and in those who never had prolonged exposure to secondhand smoke.
When you inhale cigarette smoke, which is full of cancer-causing substances (carcinogens), changes in the lung tissue begin almost immediately. At first your body may be able to repair this damage. But with each repeated exposure, normal cells that line your lungs are increasingly damaged. Over time, the damage causes cells to act abnormally and eventually cancer may develop.
The two general types of lung cancer include:
- Small cell lung cancer. Small cell lung cancer occurs almost exclusively in heavy smokers and is less common than non-small cell lung cancer.
- Non-small cell lung cancer. Non-small cell lung cancer is an umbrella term for several types of lung cancers that behave in a similar way. Non-small cell lung cancers include squamous cell carcinoma, adenocarcinoma and large cell carcinoma.
A number of factors may increase your risk of lung cancer. Some risk factors can be controlled, for instance, by quitting smoking. And other factors can't be controlled, such as your family history. Risk factors for lung cancer include:
- Smoking. Your risk of lung cancer increases with the number of cigarettes you smoke each day and the number of years you have smoked. Quitting at any age can significantly lower your risk of developing lung cancer.
- Exposure to secondhand smoke. Even if you don't smoke, your risk of lung cancer increases if you're exposed to secondhand smoke.
- Exposure to radon gas. Radon is produced by the natural breakdown of uranium in soil, rock and water that eventually becomes part of the air you breathe. Unsafe levels of radon can accumulate in any building, including homes. Radon testing kits, which can be purchased at home improvement stores, can determine whether levels are safe.
- Exposure to asbestos and other chemicals. Workplace exposure to asbestos and other substances known to cause cancer — such as arsenic, chromium and nickel — also can increase your risk of developing lung cancer, especially if you're a smoker.
- Family history of lung cancer. People with a parent, sibling or child with lung cancer have an increased risk of the disease.
Lung cancer can cause complications, such as:
- Shortness of breath. People with lung cancer can experience shortness of breath if cancer grows to block the major airways. Lung cancer can also cause fluid to accumulate around the lungs, making it harder for the affected lung to expand fully when you inhale.
- Coughing up blood. Lung cancer can cause bleeding in the airway, which can cause you to cough up blood (hemoptysis).
- Pain. Advanced lung cancer that spreads to the lining of a lung or to another area of the body, such as a bone, can cause pain.
- Fluid in the chest (pleural effusion). Lung cancer can cause fluid to accumulate in the space that surrounds the affected lung in the chest cavity.
- Cancer that spreads to other parts of the body (metastasis). Lung cancer often spreads (metastasizes) to other parts of the body, such as the brain and the bones.
Several organizations recommend people with an increased risk of lung cancer consider annual computerized tomography (CT) scans to look for lung cancer. If you're 55 or older and smoke or used to smoke, talk with your doctor about the benefits and risks of lung cancer screening.
If there's reason to think that you may have lung cancer, your doctor can order a number of tests to look for cancerous cells and to rule out other conditions. In order to diagnose lung cancer, your doctor may recommend:
- Imaging tests. An X-ray image of your lungs may reveal an abnormal mass or nodule. A CT scan can reveal small lesions in your lungs that might not be detected on an X-ray.
- Sputum cytology. If you have a cough and are producing sputum, looking at the sputum under the microscope can sometimes reveal the presence of lung cancer cells.
- Tissue sample (biopsy). A sample of abnormal cells may be removed in a procedure called a biopsy. Your doctor can perform a biopsy in a number of ways, including bronchoscopy, in which your doctor examines abnormal areas of your lungs using a lighted tube that's passed down your throat and into your lungs; mediastinoscopy, in which an incision is made at the base of your neck and surgical tools are inserted behind your breastbone to take tissue samples from lymph nodes; and needle biopsy, in which your doctor uses X-ray or CT images to guide a needle through your chest wall and into the lung tissue to collect suspicious cells. A biopsy sample may also be taken from lymph nodes or other areas where cancer has spread, such as your liver.
You and your doctor choose a cancer treatment plan based on a number of factors, such as your overall health, the type and stage of your cancer, and your preferences. Options typically include one or more treatments, including surgery, chemotherapy, radiation therapy or targeted drug therapy.
Surgery removes the lung cancer and a margin of healthy tissue. If you undergo surgery, your surgeon may also remove lymph nodes from your chest in order to check them for signs of cancer.
Chemotherapy uses drugs to kill cancer cells. One or more chemotherapy drugs may be given through a vein in your arm (intravenously) or taken orally. A combination of drugs usually is given in a series of treatments over a period of weeks or months, with breaks in between so that you can recover. Chemotherapy is often used after surgery to kill any cancer cells that may remain. It may also be used before surgery to shrink cancers and make them easier to remove. In some cases, chemotherapy can be used to relieve pain and other symptoms of advanced cancer.
Radiation therapy uses high-powered energy beams, such as X-rays, to kill cancer cells. Radiation therapy can be directed at your lung cancer from outside your body or it can be put inside needles, seeds or catheters and placed inside your body near the cancer. Radiation therapy can be used after surgery to kill any cancer cells that may remain. It may also be used as the first treatment for lung cancers that can't be removed during surgery. For people with advanced lung cancer, radiation therapy may be used to relieve pain and other symptoms.
Targeted therapies are newer cancer treatments that work by targeting specific abnormalities in cancer cells.
- Bevacizumab (Avastin). Bevacizumab stops a tumor from creating a new blood supply. Blood vessels that connect to tumors can supply oxygen and nutrients to the tumor, allowing it to grow.
- Erlotinib (Tarceva). Erlotinib blocks chemicals that signal the cancer cells to grow and divide.
- Crizotinib (Xalkori). Crizotinib blocks chemicals that allow cancer cells to grow out of control and live longer than normal cells.
Clinical trials are studies of experimental lung cancer treatments. You may be interested in enrolling in a clinical trial if lung cancer treatments aren't working or if your treatment options are limited. The treatments studied in a clinical trial may be the latest innovations, but they don't guarantee a cure.
Many people with lung cancer experience shortness of breath at some point in the course of the disease. Treatments, such as supplemental oxygen, and medications are available to help you feel more comfortable
To cope with shortness of breath, it may help to:
- Try to relax. Feeling short of breath can be scary. But fear and anxiety only make it harder to breathe. When you begin to feel short of breath, try to manage the fear by choosing an activity that helps you relax. Listen to music, imagine your favorite vacation spot, meditate or say a prayer.
- Find a comfortable position. It may help to lean forward when you feel short of breath.
- Focus on your breath. When you feel short of breath, focus your mind on your breathing. Instead of trying to fill your lungs with air, concentrate on moving the muscles that control your diaphragm. Try breathing through pursed lips and pacing your breaths with your activity.
- Save your energy for what's important. If you're short of breath, you may become tired easily. Cut out the nonessential tasks from your day so that you can save your energy for what needs to be done.
A diagnosis of cancer can be overwhelming. With time you'll find ways to cope with the distress and uncertainty of cancer. Until then, you may find it helps to:
- Learn enough about lung cancer to make decisions about your care. As you learn more about lung cancer, you may become more confident in making treatment decisions.
- Keep friends and family close. Keeping your close relationships strong will help you deal with your lung cancer. Friends and family can provide the practical support you'll need, such as helping take care of your house if you're in the hospital. And they can serve as emotional support when you feel overwhelmed by cancer.
- Find someone to talk with. Find a good listener who is willing to listen to you talk about your hopes and fears. This may be a friend or family member. The concern and understanding of a counselor, medical social worker, clergy member or cancer support group also may be helpful.
There's no sure way to prevent lung cancer, but you can reduce your risk if you:
- Don't smoke. If you've never smoked, don't start. Talk to your children about not smoking so that they can understand how to avoid this major risk factor for lung cancer. Begin conversations about the dangers of smoking with your children early so that they know how to react to peer pressure.
- Stop smoking. Stop smoking now. Quitting reduces your risk of lung cancer, even if you've smoked for years. Talk to your doctor about strategies and stop-smoking aids that can help you quit. Options include nicotine replacement products, medications and support groups.
- Avoid secondhand smoke. If you live or work with a smoker, urge him or her to quit. At the very least, ask him or her to smoke outside. Avoid areas where people smoke, such as bars and restaurants, and seek out smoke-free options.
- Test your home for radon. Have the radon levels in your home checked, especially if you live in an area where radon is known to be a problem. High radon levels can be remedied to make your home safer. For information on radon testing, contact your local department of public health or a local chapter of the American Lung Association.
- Avoid carcinogens at work. Take precautions to protect yourself from exposure to toxic chemicals at work. Follow your employer's precautions. For instance, if you're given a face mask for protection, always wear it. Ask your doctor what more you can do to protect yourself at work. Your risk of lung damage from workplace carcinogens increases if you smoke.
- Eat a diet full of fruits and vegetables. Choose a healthy diet with a variety of fruits and vegetables.
- Exercise most days of the week. If you don't exercise regularly, start out slowly. Try to exercise most days of the week.