Irritable bowel syndrome (IBS) is a common disorder that affects the large intestine (colon). Irritable bowel syndrome commonly causes cramping, abdominal pain, bloating, gas, diarrhea and constipation. IBS is a chronic condition that you will need to manage long term.
Even though signs and symptoms are uncomfortable, IBS — unlike ulcerative colitis and Crohn's disease, which are forms of inflammatory bowel disease — doesn't cause changes in bowel tissue or increase your risk of colorectal cancer.
Only a small number of people with irritable bowel syndrome have severe signs and symptoms. Some people can control their symptoms by managing diet, lifestyle and stress. Others will need medication and counseling.
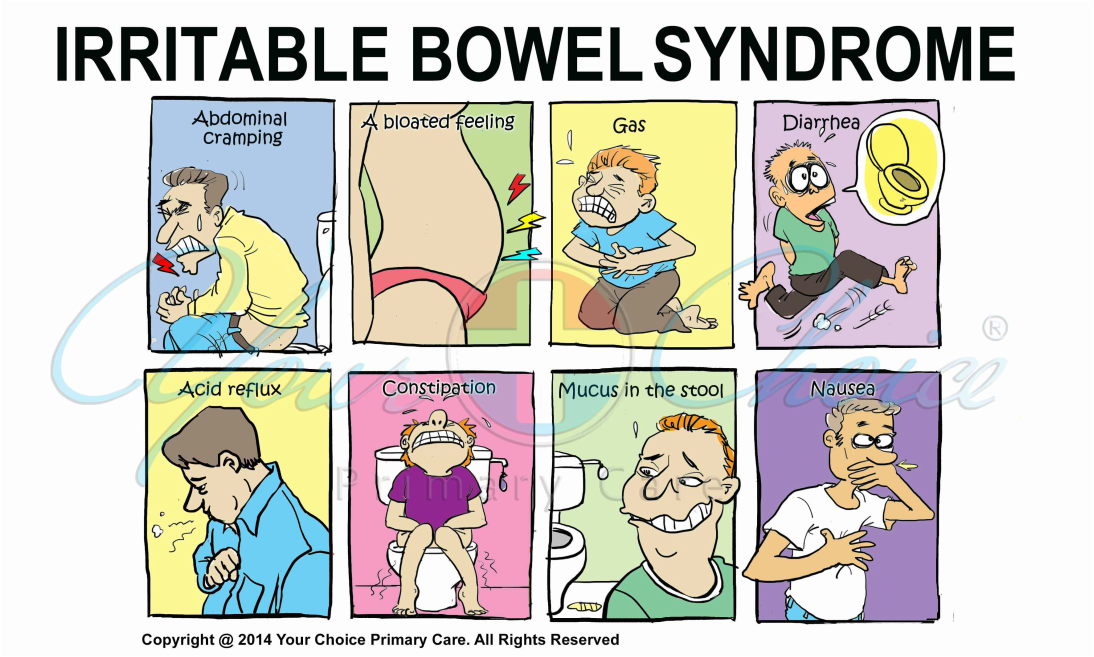
The signs and symptoms of irritable bowel syndrome can vary widely from person to person and often resemble those of other diseases. Among the most common are:
- Abdominal pain or cramping
- A bloated feeling
- Gas
- Diarrhea or constipation — sometimes alternating bouts of constipation and diarrhea
- Mucus in the stool
For most people, IBS is a chronic condition, although there will likely be times when the signs and symptoms are worse and times when they improve or even disappear completely.
When to see a doctor
Although as many as 1 in 5 American adults has signs and symptoms of irritable bowel syndrome, fewer than 1 in 5 who have symptoms seek medical help. Yet it's important to see your doctor if you have a persistent change in bowel habits or if you have any other signs or symptoms of IBS because these may indicate a more serious condition, such as colon cancer.
Symptoms that may indicate a more serious condition include:
- Rectal bleeding
- Abdominal pain that progresses or occurs at night
- Weight loss
Your doctor may be able to help you find ways to relieve symptoms as well as rule out other conditions, such as inflammatory bowel disease and colon cancer. Your doctor can also help you avoid possible complications from problems such as chronic diarrhea.
It's not known exactly what causes irritable bowel syndrome, but a variety of factors play a role. The walls of the intestines are lined with layers of muscle that contract and relax in a coordinated rhythm as they move food from your stomach through your intestinal tract to your rectum. If you have irritable bowel syndrome, the contractions may be stronger and last longer than normal, causing gas, bloating and diarrhea. Or the opposite may occur, with weak intestinal contractions slowing food passage and leading to hard, dry stools.
Abnormalities in your gastrointestinal nervous system also may play a role, causing you to experience greater than normal discomfort when your abdomen stretches from gas or stool. Poorly coordinated signals between the brain and the intestines can make your body overreact to the changes that normally occur in the digestive process. This overreaction can cause pain, diarrhea or constipation.
Triggers vary from person to person. Stimuli that don't bother other people can trigger symptoms in people with IBS — but not all people with the condition react to the same stimuli. Common triggers include:
- Foods. The role of food allergy or intolerance in irritable bowel syndrome is not yet clearly understood, but many people have more severe symptoms when they eat certain things. A wide range of foods has been implicated — chocolate, spices, fats, fruits, beans, cabbage, cauliflower, broccoli, milk, carbonated beverages and alcohol to name a few.
- Stress. Most people with IBS find that their signs and symptoms are worse or more frequent during periods of increased stress, such as finals week or the first weeks on a new job.
- Hormones. Because women are twice as likely to have IBS, researchers believe that hormonal changes play a role in this condition. Many women find that signs and symptoms are worse during or around their menstrual periods.
- Other illnesses. Sometimes another illness, such as an acute episode of infectious diarrhea (gastroenteritis) or too many bacteria in the intestines (bacterial overgrowth), can trigger IBS.
Many people have occasional signs and symptoms of irritable bowel syndrome, but you're more likely to have IBS if you:
- Are young. IBS tends to occur in people under age 45.
- Are female. Overall, about twice as many women as men have the condition.
- Have a family history of IBS. Studies suggest that people who have a family member with IBS may be at increased risk of the condition.
- Have a mental health problem. Anxiety, depression, a personality disorder and a history of childhood sexual abuse are risk factors. For women, domestic abuse may be a risk factor as well.
Diarrhea and constipation, both signs of irritable bowel syndrome, can aggravate hemorrhoids. In addition, if you avoid certain foods, you may not get enough of the nutrients you need, leading to malnourishment. But the condition's impact on your overall quality of life may be the most significant complication. These effects of IBS may cause you to feel you're not living life to the fullest, leading to discouragement or depression.
Make an appointment with your primary care doctor if you have symptoms of IBS. After an initial evaluation, your doctor may refer you to a specialist in digestive disorders (gastroenterologist) for more extensive testing.
What you can do
While you wait for your appointment, check with your family members to find out if any relatives have been diagnosed with inflammatory bowel disease or colon cancer. In addition, start jotting down notes about how often your symptoms occur and any factors that seem to trigger their occurrence.
Some red flag signs and symptoms that suggest a need for additional testing include:
- New onset after age 50
- Weight loss
- Rectal bleeding
- Fever
- Nausea or recurrent vomiting
- Abdominal pain, especially if it's not completely relieved by a bowel movement, or occurs at night
- Diarrhea that is persistent or awakens you from sleep
- Anemia related to low iron
If you fit the IBS criteria and don't have any red flag signs or symptoms, your doctor may suggest a course of treatment without doing additional testing. But if you don't respond to that treatment, you'll likely require more tests.
Imaging tests:
- Flexible sigmoidoscopy. This test examines the lower part of the colon (sigmoid) with a flexible, lighted tube (sigmoidoscope).
- Colonoscopy. In some cases, especially if you are age 50 or older or have other signs of a potentially more serious condition, your doctor may perform this diagnostic test in which a small, flexible tube is used to examine the entire length of the colon.
- Computerized tomography (CT) scan. CT scans produce cross-sectional X-ray images of internal organs. CT scans of your abdomen and pelvis may help your doctor rule out other causes of your symptoms, especially if you have abdominal pain.
Laboratory tests:
- Lactose intolerance tests. Lactase is an enzyme you need to digest the sugar found in dairy products. If you don't produce this enzyme, you may have problems similar to those caused by irritable bowel syndrome, including abdominal pain, gas and diarrhea. To find out if this is the cause of your symptoms, your doctor may ask you to remove milk and milk products from your diet for several weeks.
- Breath tests. Your doctor may perform a breath test to look for a condition called bacterial overgrowth, in which bacteria from the colon grow up into the small intestine, leading to bloating, abdominal discomfort and diarrhea. This is more common among people who have had bowel surgery or who have diabetes or some other disease that slows down digestion.
- Blood tests. Celiac disease is sensitivity to wheat, barley and rye protein that may cause signs and symptoms like those of irritable bowel syndrome. Blood tests can help rule out this disorder. Children with IBS have a far greater risk of celiac disease than do children who don't have IBS. If your doctor suspects that you have celiac disease, he or she may perform an upper endoscopy to obtain a biopsy of your small intestine.
- Stool tests. If you have chronic diarrhea, doctors may want to examine your stool for bacteria or parasites.
Because it's not clear what causes irritable bowel syndrome, treatment focuses on the relief of symptoms so that you can live as normally as possible.
In most cases, you can successfully control mild signs and symptoms of irritable bowel syndrome by learning to manage stress and making changes in your diet and lifestyle. Try to avoid foods that trigger your symptoms. Also try to get enough exercise, drink plenty of fluids and get enough sleep.
Dietary changes:
- Eliminating high-gas foods. If you have bothersome bloating or are passing considerable amounts of gas, your doctor may suggest that you cut out such items as carbonated beverages, vegetables — especially cabbage, broccoli and cauliflower — and raw fruits.
- Eliminating gluten. Research shows that some people with IBS report improvement in diarrhea symptoms if they stop eating gluten (wheat, barley and rye).
- Eliminating FODMAPs. Some people are sensitive to types of carbohydrates such as fructose, fructans, lactose and others, called FODMAPs (fermentable oligo-, di-, and monosaccharides and polyols). FODMAPs are found in certain grains, vegetables, fruits and dairy products. However, often people are not bothered by every FODMAP food. You may be able to get relief from your IBS symptoms on a strict low FODMAP diet and then reintroduce foods one at time.
Medications:
- Fiber supplements. Taking fiber supplements, such as psyllium (Metamucil) or methylcellulose (Citrucel), with fluids may help control constipation. Fiber obtained from food may cause much more bloating compared with a fiber supplement.
- Anti-diarrheal medications. Over-the-counter medications, such as loperamide (Imodium), can help control diarrhea.
- Anticholinergic and antispasmodic medications. These medications, such as hyoscyamine (Levsin) and dicyclomine (Bentyl), can help relieve painful bowel spasms.
- Antidepressant medications. If your symptoms include pain or depression, your doctor may recommend a tricyclic antidepressant or a selective serotonin reuptake inhibitor (SSRI). These medications help relieve depression as well as inhibit the activity of neurons that control the intestines.
- Antibiotics. Some people whose symptoms are due to an overgrowth of bacteria in their intestines may benefit from antibiotic treatment.
- Counseling. You may benefit from counseling if you have depression or if stress tends to worsen your symptoms.
- Lubiprostone (Amitiza). Lubiprostone works by increasing fluid secretion in your small intestine to help with the passage of stool. Common side effects include nausea, diarrhea and abdominal pain. Lubiprostone is generally prescribed only for whom other treatments haven't been successful.
In many cases, simple changes in your diet and lifestyle can provide relief from irritable bowel syndrome. Although your body may not respond immediately to these changes, your goal is to find long-term, not temporary, solutions:
- Experiment with fiber. When you have irritable bowel syndrome, fiber can be a mixed blessing. Although it helps reduce constipation, it can also make gas and cramping worse. The best approach is to slowly increase the amount of fiber in your diet over a period of weeks. Examples of foods that contain fiber are whole grains, fruits, vegetables and beans. If your signs and symptoms remain the same or worse, tell your doctor. You may also want to talk to a dietitian. Some people do better limiting dietary fiber and instead take a fiber supplement that causes less gas and bloating. If you take a fiber supplement, such as Metamucil or Citrucel, be sure to introduce it slowly and drink plenty of water every day to reduce gas, bloating and constipation. If you find that taking fiber helps your IBS, use it on a regular basis for best results.
- Avoid problem foods. If certain foods make your signs and symptoms worse, don't eat them. These may include alcohol, chocolate, caffeinated beverages such as coffee and sodas, medications that contain caffeine, dairy products, and sugar-free sweeteners such as sorbitol or mannitol. If gas is a problem for you, foods that might make symptoms worse include beans, cabbage, cauliflower and broccoli. Fatty foods also may be a problem for some people. Chewing gum or drinking through a straw can lead to swallowing air, causing more gas.
- Eat at regular times. Don't skip meals, and try to eat about the same time each day to help regulate bowel function. If you have diarrhea, you may find that eating small, frequent meals makes you feel better. But if you're constipated, eating larger amounts of high-fiber foods may help move food through your intestines.
- Take care with dairy products. If you're lactose intolerant, try substituting yogurt for milk. Or use an enzyme product to help break down lactose. Consuming small amounts of milk products or combining them with other foods also may help. In some cases, though, you may need to stop eating dairy foods completely. If so, be sure to get enough protein, calcium and B vitamins from other sources.
- Drink plenty of liquids. Try to drink plenty of fluids every day. Water is best. Alcohol and beverages that contain caffeine stimulate your intestines and can make diarrhea worse, and carbonated drinks can produce gas.
- Exercise regularly. Exercise helps relieve depression and stress, stimulates normal contractions of your intestines, and can help you feel better about yourself. If you've been inactive, start slowly and gradually increase the amount of time you exercise. If you have other medical problems, check with your doctor before starting an exercise program.
- Use anti-diarrheal medications and laxatives with caution. If you try over-the-counter anti-diarrheal medications, such as Imodium or Kaopectate, use the lowest dose that helps. Imodium may be helpful if taken 20 to 30 minutes before eating, especially if you know that the food planned for your meal is likely to cause diarrhea.
- Herbs. Peppermint is a natural antispasmodic that relaxes smooth muscles in the intestines. Peppermint may provide short-term relief of IBS symptoms, but study results have been inconsistent. If you'd like to try peppermint, be sure to use enteric-coated capsules. Peppermint may make heartburn worse. Before taking any herbs, check with your doctor to be sure they won't interact or interfere with other medications. A blend of herbs called STW 5 (Iberogast) has been shown to help some people.
- Hypnosis. Hypnosis may reduce abdominal pain and bloating. A trained professional teaches you how to enter a relaxed state and then guides you in relaxing your abdominal muscles.
- Probiotics. Probiotics are "good" bacteria that normally live in your intestines and are found in certain foods, such as yogurt, and in dietary supplements. It's been suggested that if you have irritable bowel syndrome, you may not have enough good bacteria and that adding probiotics to your diet may help ease your symptoms. Recent studies suggest that certain probiotics may relieve symptoms of IBS, such as abdominal pain, bloating, diarrhea and quality of life, although additional investigation is needed.
- Regular exercise, yoga, massage or meditation. These can all be useful ways to relieve stress. You can take classes in yoga and meditation or practice at home using books or videos.
Living with irritable bowel syndrome presents daily challenges. It may be painful or embarrassing and can seriously affect the quality of your life. These suggestions may help you cope more easily:
- Learn as much about IBS as you can. Talk to your doctor, look for information on the Internet from reputable sources such as the National Institutes of Health, and read books and pamphlets. Being informed about your condition can help you take better charge of it.
- Identify the factors that trigger IBS. This is a key step both in managing your condition and in helping you feel you have control of your life.
- Seek out others with IBS. Talking to people who know what you're going through can be reassuring. Try IBS support groups on the Internet or in your community.
- Counseling. In some cases, a psychologist or psychiatrist can help you learn to reduce stress by looking at how you respond to events and then working with you to modify or change that response.
- Biofeedback. This stress-reduction technique helps you reduce muscle tension and slow your heart rate with the feedback help of a machine. You're then taught how to produce these changes yourself. The goal is to help you enter a relaxed state so that you can cope more easily with stress.
- Progressive relaxation exercises. These help you relax muscles in your body, one by one. Start by tightening the muscles in your feet, then concentrate on slowly letting all of the tension go. Next, tighten and relax your calves. Continue until the muscles in your body, including those in your eyes and scalp, are relaxed.
- Deep breathing. Most adults breathe from their chests. But you become calmer when you breathe from your diaphragm, the muscle that separates your chest from your abdomen. When you inhale, allow your belly to expand. When you exhale, your belly naturally contracts. Deep breathing can also help relax your abdominal muscles, which may lead to more-normal bowel activity.
- Mindfulness training. This stress-reduction technique helps you focus on being in the moment and letting go of worries and distractions.
- Other techniques. Set aside at least 20 minutes a day for any activity you find relaxing — listening to music, reading, playing computer games or just soaking in a warm bath.