Heart failure, sometimes known as congestive heart failure, occurs when your heart muscle doesn't pump blood as well as it should. Certain conditions, such as narrowed arteries in your heart (coronary artery disease) or high blood pressure, gradually leave your heart too weak or stiff to fill and pump efficiently.
Not all conditions that lead to heart failure can be reversed, but treatments can improve the signs and symptoms of heart failure and help you live longer. Lifestyle changes — such as exercising, reducing salt in your diet, managing stress and losing weight — can improve your quality of life.
One way to prevent heart failure is to control conditions that cause heart failure, such as coronary artery disease, high blood pressure, diabetes or obesity.
Heart failure can be ongoing (chronic), or your condition may start suddenly (acute).
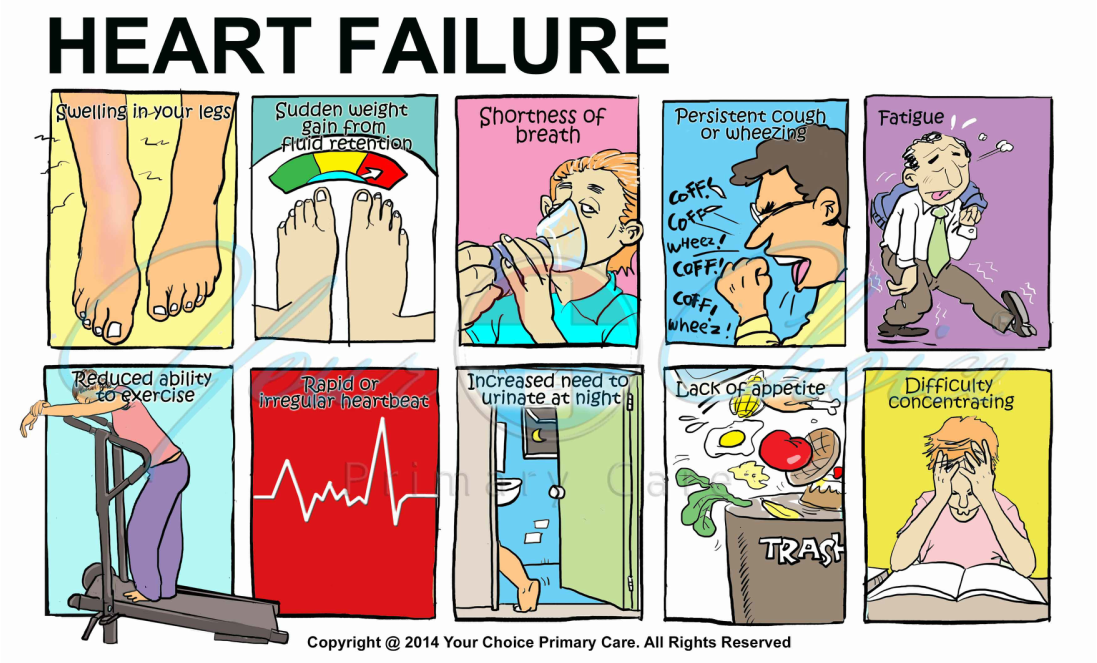
Heart failure signs and symptoms may include:
- Shortness of breath (dyspnea) when you exert yourself or when you lie down
- Fatigue and weakness
- Swelling (edema) in your legs, ankles and feet
- Rapid or irregular heartbeat
- Reduced ability to exercise
- Persistent cough or wheezing with white or pink blood-tinged phlegm
- Increased need to urinate at night
- Swelling of your abdomen (ascites)
- Sudden weight gain from fluid retention
- Lack of appetite and nausea
- Difficulty concentrating or decreased alertness
- Sudden, severe shortness of breath and coughing up pink, foamy mucus
- Chest pain if your heart failure is caused by a heart attack
When to see a doctor
See your primary care doctor if you think you might be experiencing signs or symptoms of heart failure.
Seek emergency treatment if you experience any of the following:
- Chest pain
- Fainting or severe weakness
- Rapid or irregular heartbeat associated with shortness of breath, chest pain or fainting
- Sudden, severe shortness of breath and coughing up pink, foamy mucus
Although these signs and symptoms may be due to heart failure, there are many other possible causes, including other life-threatening heart and lung conditions. Don't try to diagnose yourself. Call 911 or your local emergency number for immediate help. Emergency room health care providers will try to stabilize your condition and determine if your symptoms are due to heart failure or something else.
If you have a diagnosis of heart failure and if any of the symptoms suddenly become worse or you develop a new sign or symptom, it may mean that existing heart failure is getting worse or not responding to treatment. Contact your cardiologist promptly.
Heart failure often develops after other conditions have damaged or weakened your heart. However, the heart doesn't need to be weakened to cause heart failure. It can also occur if the heart becomes too stiff.
In heart failure, the main pumping chambers of your heart (the ventricles) may become stiff and not fill properly between beats. In some cases of heart failure, your heart muscle may become damaged and weakened, and the ventricles stretch (dilate) to the point that the heart can't pump blood efficiently throughout your body. Over time, the heart can no longer keep up with the normal demands placed on it to pump blood to the rest of your body.
An ejection fraction is an important measurement of how well your heart is pumping and is used to help classify heart failure and guide treatment. In a healthy heart, the ejection fraction is 50 percent or higher — meaning that more than half of the blood that fills the ventricle is pumped out with each beat. But heart failure can occur even with a normal ejection fraction. This happens if the heart muscle becomes stiff from conditions such as high blood pressure.
Any of the following conditions can damage or weaken your heart and can cause heart failure. Some of these can be present without your knowing it:
- Coronary artery disease and heart attack. Coronary artery disease is the most common form of heart disease and the most common cause of heart failure. Over time, arteries that supply blood to your heart muscle narrow from a buildup of fatty deposits — a process called atherosclerosis. The buildup of plaques can cause reduced blood flow to your heart. A heart attack occurs if plaques formed by the fatty deposits in your arteries rupture. This causes a blood clot to form, which may block blood flow to an area of the heart muscle, weakening the heart's pumping ability and often leaving permanent damage. If the damage is significant, it can lead to a weakened heart muscle.
- High blood pressure (hypertension). Blood pressure is the force of blood pumped by your heart through your arteries. If your blood pressure is high, your heart has to work harder than it should to circulate blood throughout your body. Over time, the heart muscle may become thicker to compensate for the extra work it must perform. Eventually, your heart muscle may become either too stiff or too weak to effectively pump blood.
- Faulty heart valves. The valves of your heart keep blood flowing in the proper direction through the heart. A damaged valve — due to a heart defect, coronary artery disease or heart infection — forces your heart to work harder to keep blood flowing as it should. Over time, this extra work can weaken your heart. Faulty heart valves, however, can be fixed or replaced if found in time.
- Damage to the heart muscle (cardiomyopathy). Heart muscle damage (cardiomyopathy) can have many causes, including several diseases, infections, alcohol abuse and the toxic effect of drugs, such as cocaine or some drugs used for chemotherapy. Genetic factors also play an important role in several types of cardiomyopathy.
- Myocarditis. Myocarditis is an inflammation of the heart muscle. It's most commonly caused by a virus.
- Heart defects you're born with (congenital heart defects). If your heart and its chambers or valves haven't formed correctly, the healthy parts of your heart have to work harder to pump blood through your heart, which, in turn, may lead to heart failure.
- Abnormal heart rhythms (heart arrhythmias). Abnormal heart rhythms may cause your heart to beat too fast, which creates extra work for your heart. Over time, your heart may weaken, leading to heart failure. A slow heartbeat may prevent your heart from getting enough blood out to the body and may also lead to heart failure.
- Other diseases. Chronic diseases — such as diabetes, HIV, hyperthyroidism, hypothyroidism, or a buildup of iron (hemochromatosis) or protein (amyloidosis) —also may contribute to heart failure.
Risk factors include:
- High blood pressure. Your heart works harder than it has to if your blood pressure is high.
- Coronary artery disease. Narrowed arteries may limit your heart's supply of oxygen-rich blood, resulting in weakened heart muscle.
- Heart attack. Damage to your heart muscle from a heart attack may mean your heart can no longer pump as well as it should.
- Diabetes. Having diabetes increases your risk of high blood pressure and coronary artery disease.
- Some diabetes medications. The diabetes drugs rosiglitazone (Avandia) and pioglitazone (Actos) have been found to increase the risk of heart failure in some people. Don't stop taking these medications on your own, though. If you're taking them, discuss with your doctor whether you need to make any changes.
- Sleep apnea. The inability to breathe properly while you sleep at night results in low blood oxygen levels and increased risk of abnormal heart rhythms. Both of these problems can weaken the heart.
- Congenital heart defects. Some people who develop heart failure were born with structural heart defects.
- Valvular heart disease. People with valvular heart disease have a higher risk of heart failure.
- Viruses. A viral infection may have damaged your heart muscle.
- Alcohol use. Drinking too much alcohol can weaken heart muscle and lead to heart failure.
- Tobacco use. Using tobacco can increase your risk of heart failure.
- Obesity. People who are obese have a higher risk of developing heart failure.
- Irregular heartbeats. These abnormal rhythms, especially if they are very frequent and fast, can weaken the heart muscle and cause heart failure.
If you have heart failure, your outlook depends on the cause and the severity, your overall health, and other factors such as your age. Complications can include:
- Kidney damage or failure. Heart failure can reduce the blood flow to your kidneys, which can eventually cause kidney failure if left untreated. Kidney damage from heart failure can require dialysis for treatment.
- Heart valve problems. The valves of your heart, which keep blood flowing in the proper direction through your heart, may not function properly if your heart is enlarged or if the pressure in your heart is very high due to heart failure.
- Heart rhythm problems. Heart rhythm problems (arrhythmias) can be a potential complication of heart failure.
- Liver damage. Heart failure can lead to a buildup of fluid that puts too much pressure on the liver. This fluid backup can lead to scarring, which makes it more difficult for your liver to function properly.
Some people's symptoms and heart function will improve with proper treatment. However, heart failure can be life-threatening. People with heart failure may have severe symptoms, and some may require heart transplantation or support with a ventricular assist device.
If you think you may have heart failure or you are worried about your heart failure risk because of other underlying conditions, make an appointment with your primary care doctor. If heart failure is found early, your treatment may be easier and more effective. Because appointments can be brief, and because there's often a lot to discuss, it's a good idea to be prepared for your appointment. Here's some information to help you get ready for your appointment and know what to expect from your doctor.
What you can do
- Be aware of any pre-appointment restrictions. At the time you make the appointment, be sure to ask if there's anything you need to do in advance, such as restrict your diet. For some imaging tests, for example, you may need to fast for a period of time beforehand.
- Write down any symptoms you're experiencing, including any that may seem unrelated to heart failure.
- Write down key personal information, including a family history of heart disease, stroke, high blood pressure or diabetes, and any major stresses or recent life changes. Find out if anyone in your family has had heart failure. Some heart conditions that cause heart failure run in families. Knowing as much as you can about your family history can be important.
- Make a list of all medications, vitamins or supplements that you're taking.
- It's never too early to make healthy lifestyle changes, such as quitting smoking, cutting down on salt and eating healthy foods. These changes can help prevent heart failure from starting or worsening.
To diagnose heart failure, your doctor will take a careful medical history, review your symptoms and perform a physical examination. Your doctor will also check for the presence of risk factors, such as high blood pressure, coronary artery disease or diabetes. After the physical exam, your doctor may also order some of these tests:
- Blood tests. Your doctor may take a sample of your blood to check your kidney, liver and thyroid function and to look for indicators of other diseases that affect the heart. A blood test to check for a chemical called N-terminal pro-B-type natriuretic peptide (NT-proBNP) may help in diagnosing heart failure if the diagnosis isn't certain when used in addition to other tests.
- Chest X-ray. X-ray images help your doctor see the condition of your lungs and heart. In heart failure, your heart may appear enlarged and fluid buildup may be visible in your lungs. Your doctor can also use an X-ray to diagnose conditions other than heart failure that may explain your signs and symptoms.
- Electrocardiogram (ECG). This test records the electrical activity of your heart through electrodes attached to your skin. Impulses are recorded as waves and displayed on a monitor or printed on paper. This test helps your doctor diagnose heart rhythm problems and damage to your heart from a heart attack that may be underlying heart failure.
- Echocardiogram. An important test for diagnosing heart failure is the echocardiogram. An echocardiogram helps distinguish systolic heart failure from diastolic heart failure in which the heart is stiff and can't fill properly. An echocardiogram uses sound waves to produce a video image of your heart. This test can help doctors see the size and shape of your heart and how well your heart is pumping. The echocardiogram also can help doctors look for valve problems or evidence of previous heart attacks, other heart abnormalities, and some unusual causes of heart failure. Your ejection fraction is also measured during an echocardiogram.
- Stress test. Stress tests measure how your heart and blood vessels respond to exertion. You may walk on a treadmill or pedal a stationary bike while attached to an ECG machine. Or you may receive a drug intravenously that stimulates your heart similar to exercise. Stress tests help doctors see if you have coronary artery disease. Stress tests also determine how well your body is responding to your heart's decreased pumping effectiveness and can help guide long-term treatment decisions. If your doctor also wants to see images of your heart while you're exercising, he or she may order a nuclear stress test or a stress echocardiogram. It's similar to an exercise stress test, but it also uses imaging techniques to visualize your heart during the test.
- Cardiac computerized tomography (CT) scan or magnetic resonance imaging (MRI). These tests can be used to diagnose heart problems, including causes of heart failure. In a cardiac CT scan, you lie on a table inside a doughnut-shaped machine. An X-ray tube inside the machine rotates around your body and collects images of your heart and chest. In a cardiac MRI, you lie on a table inside a long tube-like machine that produces a magnetic field. The magnetic field aligns atomic particles in some of your cells. When radio waves are broadcast toward these aligned particles, they produce signals that vary according to the type of tissue they are. The signals create images of your heart.
- Coronary angiogram. In this test, a thin, flexible tube (catheter) is inserted into a blood vessel at your groin or in your arm and guided through the aorta into your coronary arteries. A dye injected through the catheter makes the arteries supplying your heart visible on an X-ray. This test helps doctors identify narrowed arteries to your heart (coronary artery disease) that can be a cause of heart failure.
Doctors sometimes can correct heart failure by treating the underlying cause. For example, repairing a heart valve or controlling a fast heart rhythm may reverse heart failure. But for most people, the treatment of heart failure involves a balance of the right medications and, in some cases, use of devices that help the heart beat and contract properly.
Medications
Doctors usually treat heart failure with a combination of medications. Depending on your symptoms, you might take one or more medications, including:
- Angiotensin-converting enzyme (ACE) inhibitors. These drugs help people with systolic heart failure live longer and feel better. ACE inhibitors are a type of vasodilator, a drug that widens blood vessels to lower blood pressure, improve blood flow and decrease the workload on the heart. Examples include enalapril (Vasotec), lisinopril (Zestril) and captopril (Capoten).
- Angiotensin II receptor blockers. These drugs, which include losartan (Cozaar) and valsartan (Diovan), have many of the same benefits as ACE inhibitors. They may be an alternative for people who can't tolerate ACE inhibitors.
- Beta blockers. This class of drugs not only slows your heart rate and reduces blood pressure but also limits or reverses some of the damage to your heart if you have systolic heart failure. Examples include carvedilol (Coreg), metoprolol (Lopressor) and bisoprolol (Zebeta). These medicines reduce the risk of some abnormal heart rhythms and lessen your chance of dying unexpectedly. Beta blockers may reduce signs and symptoms of heart failure, improve heart function, and help you live longer.
- Diuretics. Often called water pills, diuretics make you urinate more frequently and keep fluid from collecting in your body. Diuretics, such as furosemide (Lasix), also decrease fluid in your lungs so you can breathe more easily. Because diuretics make your body lose potassium and magnesium, your doctor also may prescribe supplements of these minerals. If you're taking a diuretic, your doctor will likely monitor levels of potassium and magnesium in your blood through regular blood tests
- Aldosterone antagonists. These drugs include spironolactone (Aldactone) and eplerenone (Inspra). These are potassium-sparing diuretics, which also have additional properties that may help people with severe systolic heart failure live longer. Unlike some other diuretics, spironolactone and eplerenone can raise the level of potassium in your blood to dangerous levels, so talk to your doctor if increased potassium is a concern, and learn if you need to modify your intake of food that's high in potassium.
- Digoxin (Lanoxin). This drug, also referred to as digitalis, increases the strength of your heart muscle contractions. It also tends to slow the heartbeat. Digoxin reduces heart failure symptoms in systolic heart failure.
You may need to take two or more medications to treat heart failure. Your doctor may prescribe other heart medications as well — such as nitrates for chest pain, a statin to lower cholesterol or blood-thinning medications to help prevent blood clots — along with heart failure medications.
You may be hospitalized if you have a flare-up of heart failure symptoms. While in the hospital, you may receive additional medications to help your heart pump better and relieve your symptoms. You may also receive supplemental oxygen through a mask or small tubes placed in your nose. If you have severe heart failure, you may need to use supplemental oxygen long term.
In some cases, doctors recommend surgery to treat the underlying problem that led to heart failure. Some treatments being studied and used in certain people include:
- Coronary bypass surgery. If severely blocked arteries are contributing to your heart failure, your doctor may recommend coronary artery bypass surgery. In this procedure, blood vessels from your leg, arm or chest bypass a blocked artery in your heart to allow blood to flow through your heart more freely.
- Heart valve repair or replacement. If a faulty heart valve causes your heart failure, your doctor may recommend repairing or replacing the valve. Valve replacement is done when valve repair isn't possible. In valve replacement surgery, the damaged valve is replaced by an artificial (prosthetic) valve.
- Implantable cardioverter-defibrillators (ICDs). An ICD is a device similar to a pacemaker. It's implanted under the skin in your chest with wires leading through your veins and into your heart. The ICD monitors the heart rhythm. If the heart starts beating at a dangerous rhythm, or if your heart stops, the ICD tries to pace your heart or shock it back into normal rhythm. An ICD can also function as a pacemaker and speed your heart up if it is going too slow.
- Heart pumps. These mechanical devices, such as ventricular assist devices (VADs), are implanted into the abdomen or chest and attached to a weakened heart to help it pump blood to the rest of your body.
- Heart transplant. Some people have such severe heart failure that surgery or medications don't help. They may need to have their diseased heart replaced with a healthy donor heart. Heart transplants can dramatically improve the survival and quality of life of some people with severe heart failure. However, candidates for transplantation often have to wait a long time before a suitable donor heart is found.
Even with the number of treatments available for heart failure, it's possible that your heart failure may worsen to the point where medications are no longer working and a heart transplant or device isn't an option. If this occurs, you may need to enter hospice care. Hospice care provides a special course of treatment to terminally ill people.
Hospice care allows family and friends — with the aid of nurses, social workers and trained volunteers — to care for and comfort a loved one at home or in hospice residences. Hospice care provides emotional, psychological, social and spiritual support for people who are ill and those closest to them.
Although most people under hospice care remain in their own homes, the program is available anywhere — including nursing homes and assisted living centers. For people who stay in a hospital, specialists in end-of-life care can provide comfort, compassionate care and dignity.
Although it can be difficult, discuss end-of-life issues with your family and medical team. Part of this discussion will likely involve advance directives — a general term for oral and written instructions you give concerning your medical care should you become unable to speak for yourself.
If you have an implantable cardioverter-defibrillator (ICD), one important consideration to discuss with your family and doctors is turning off the defibrillator so that it can't deliver shocks to make your heart continue beating.
Making lifestyle changes can often help relieve signs and symptoms of heart failure and prevent the disease from worsening. These changes may be among the most important and beneficial you can make. Lifestyle changes your doctor may recommend include:
- Stop smoking. Smoking damages your blood vessels, raises blood pressure, reduces the amount of oxygen in your blood and makes your heart beat faster. Avoid secondhand smoke, too.
- Weight monitoring . Check weight daily. Weight gain may mean that you're retaining fluids and need a change in your treatment plan.
- Check your legs, ankles and feet for swelling daily. Check for any changes in swelling in your legs, ankles or feet daily. Check with your doctor if the swelling worsens.
- Eat a healthy diet. Aim to eat a diet that includes fruits and vegetables, whole grains, fat-free or low-fat dairy products, and lean proteins.
- Restrict salt in your diet. Too much sodium contributes to water retention, which makes your heart work harder and causes shortness of breath and swollen legs, ankles and feet.
- Maintain a healthy weight. If you're overweight, your dietitian will help you work toward your ideal weight. Even losing a small amount of weight can help.
- Consider getting vaccinations. If you have heart failure, you may want to get influenza and pneumonia vaccinations. Ask your doctor about these vaccinations.
- Limit fats and cholesterol. In addition to avoiding high-sodium foods, limit the amount of saturated fat, trans fat and cholesterol in your diet. A diet high in fat and cholesterol is a risk factor for coronary artery disease, which often underlies or contributes to heart failure.
- Limit alcohol and fluids. Your doctor likely will recommend that you don't drink alcohol if you have heart failure, since it can interact with your medication, weaken your heart muscle and increase your risk of abnormal heart rhythms. If you have severe heart failure, your doctor may also suggest you limit the amount of fluids you drink.
- Be active. Moderate aerobic activity helps keep the rest of your body healthy and conditioned, reducing the demands on your heart muscle.
- Reduce stress. When you're anxious or upset, your heart beats faster, you breathe more heavily and your blood pressure often goes up. This can make heart failure worse, since your heart is already having trouble meeting the body's demands. Find ways to reduce stress in your life. To give your heart a rest, try napping or putting your feet up when possible. Spend time with friends and family to be social and help keep stress at bay.
- Sleep easy. If you're having shortness of breath, especially at night, sleep with your head propped up using a pillow or a wedge. If you snore or have had other sleep problems, make sure you get tested for sleep apnea.
To improve your sleep at night, prop up your head with pillows. Also, discuss with your doctor changing the time for taking medications, especially diuretics. Taking diuretics earlier in the day may decrease the need to urinate as often during the night.