Cervical cancer is a type of cancer that occurs in the cells of the cervix — the lower part of the uterus that connects to the vagina.
Various strains of the human papillomavirus (HPV), a sexually transmitted infection, play a role in causing most cervical cancer. When exposed to HPV, a woman's immune system typically prevents the virus from doing harm. In a small group of women, however, the virus survives for years, contributing to the process that causes some cells on the surface of the cervix to become cancer cells.
You can reduce your risk of developing cervical cancer by having screening tests and receiving a vaccine that protects against HPV infection.
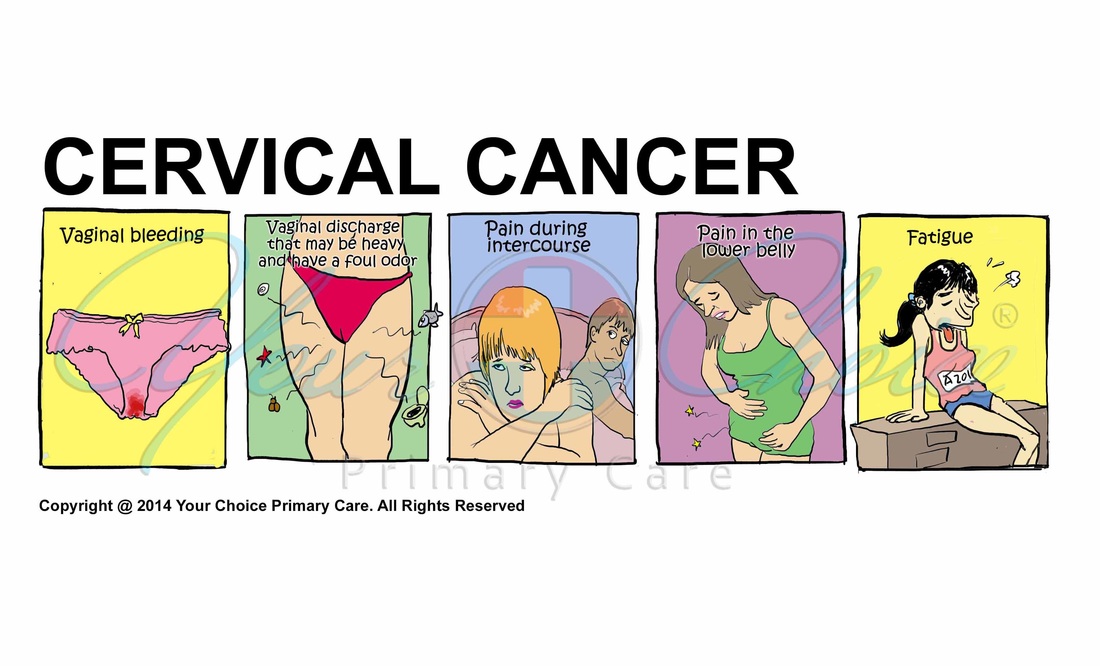
Early-stage cervical cancer generally produces no signs or symptoms. Signs and symptoms of more-advanced cervical cancer include:
- Vaginal bleeding after intercourse, between periods or after menopause
- Watery, bloody vaginal discharge that may be heavy and have a foul odor
- Pelvic pain or pain during intercourse
- Fatigue
When to see a doctor
Make an appointment with your primary care doctor if you have any signs or symptoms that concern you.
Cervical cancer begins when healthy cells acquire a genetic change (mutation) that causes them to turn into abnormal cells. Healthy cells grow and multiply at a set rate, eventually dying at a set time. Cancer cells grow and multiply out of control, and they don't die. The accumulating abnormal cells form a mass (tumor). Cancer cells invade nearby tissues and can break off from a tumor to spread (metastasize) elsewhere in the body.
Risk factors for cervical cancer include:
- Many sexual partners. The greater your number of sexual partners — and the greater your partner's number of sexual partners — the greater your chance of acquiring HPV.
- Early sexual activity. Having sex at an early age increases your risk of HPV.
- Other sexually transmitted infections (STIs). Having other STIs — such as chlamydia, gonorrhea, syphilis and HIV/AIDS — increases your risk of HPV.
- A weak immune system. You may be more likely to develop cervical cancer if your immune system is weakened by another health condition and you have HPV.
- Smoking. Smoking is associated with squamous cell cervical cancer.
Cervical cancer that is detected early is more likely to be treated successfully. Most guidelines suggest that women begin screening for cervical cancer and precancerous changes at age 21. Screening tests include:
- Pap test. During a Pap test, your doctor scrapes and brushes cells from your cervix, which are then examined in a lab for abnormalities. A Pap test can detect abnormal cells in the cervix, including cancer cells and cells that show changes that increase the risk of cervical cancer.
- HPV DNA test. The HPV DNA test involves testing cells collected from the cervix for infection with any of the types of HPV that are most likely to lead to cervical cancer. This test may be an option for women age 30 and older, or for younger women with an abnormal Pap test.
If cervical cancer is suspected, your doctor will make a referral to a gynecologist who is likely to start with a thorough examination of your cervix with a special magnifying instrument (colposcope) to check for abnormal cells. During the colposcopic examination, your doctor is likely to take a sample of cervical cells (biopsy) for laboratory testing. To obtain tissue, your doctor may use:
- Punch biopsy, which involves using a sharp tool to pinch off small samples of cervical tissue.
- Endocervical curettage, which uses a small, spoon-shaped instrument (curet) or a thin brush to scrape a tissue sample from the cervix.
If the punch biopsy or endocervical curettage is worrisome, your doctor may perform one of the following tests:
- Electrical wire loop, which uses a thin, low-voltage electrical wire to obtain a small tissue sample. Generally this is done under local anesthesia in the office.
- Cone biopsy, which is a procedure that allows your doctor to obtain deeper layers of cervical cells for laboratory testing. Cone biopsy may be done in a hospital under general anesthesia.
If your doctor determines that you have cervical cancer, you'll have further tests to determine the extent (stage) of your cancer. Your cancer's stage is a key factor in deciding on your treatment. Staging exams include:
- Imaging tests. Tests such as X-rays, CT scans, magnetic resonance imaging (MRI) and positron emission tomography (PET) help your doctor determine whether your cancer has spread beyond your cervix.
- Visual examination of your bladder and rectum. Your doctor may use special scopes to see inside your bladder and rectum.Treatment for cervical cancer depends on several factors, such as the stage of the cancer, other health problems you may have and your preferences. Surgery, radiation, chemotherapy or a combination of the three may be used.
Early-stage cervical cancer is typically treated with surgery to remove the uterus (hysterectomy). A hysterectomy can cure early-stage cervical cancer and prevent recurrence. But removing the uterus makes it impossible to become pregnant.
Radiation therapy uses high-powered energy beams, such as X-rays, to kill cancer cells. Radiation therapy may be used alone or with chemotherapy before surgery to shrink a tumor or after surgery to kill any remaining cancer cells. Premenopausal women may stop menstruating and begin menopause as a result of radiation therapy. If you might want to get pregnant after radiation treatment, ask your doctor about ways to preserve your eggs before treatment starts.
Chemotherapy uses medications, usually injected into a vein, to kill cancer cells. Low doses of chemotherapy are often combined with radiation therapy, since chemotherapy may enhance the effects of the radiation. Higher doses of chemotherapy are used to control advanced cervical cancer that may not be curable.
No one can be prepared for a cancer diagnosis. You can, however, try to manage the shock and fear you're feeling by taking steps to control what you can about your situation. Every woman deals with a cervical cancer diagnosis in her own way. With time, you'll discover what helps you cope. Until then, you can start to take control by attempting to:
- Learn enough about cervical cancer to make decisions about your care.
- Find someone to talk with. You may feel comfortable discussing your feelings with a friend or family member, or you might prefer meeting with a formal support group. Support groups for the families of cancer survivors also are available.
- Let people help. Cancer treatments can be exhausting. Let friends and family know what types of help would be most useful for you.
- Set reasonable goals. Having goals helps you feel in control and can give you a sense of purpose. But choose goals that you can reach.
- Take time for yourself. Eating well, relaxing and getting enough rest can help combat the stress and fatigue of cancer.
- Get vaccinated against HPV. The vaccine is most effective if given to girls before they become sexually active.
- Have routine Pap tests. Pap tests can detect precancerous conditions of the cervix, so they can be monitored or treated in order to prevent cervical cancer. Most medical organizations suggest women begin routine Pap tests at age 21 and repeat them at a regular interval.
- Practice safe sex. Using a condom, having fewer sexual partners and delaying intercourse may reduce your risk of cervical cancer.
- Don't smoke.