Breast cancer is cancer that forms in the cells of the breasts.
After skin cancer, breast cancer is the most common cancer diagnosed in women in the United States. Breast cancer can occur in both men and women, but it's far more common in women.
Substantial support for breast cancer awareness and research funding has helped improve the screening and diagnosis and advances in the treatment of breast cancer. Breast cancer survival rates have increased, and the number of deaths steadily has been declining, which is largely due to a number of factors such as earlier detection, a new personalized approach to treatment and a better understanding of the disease.
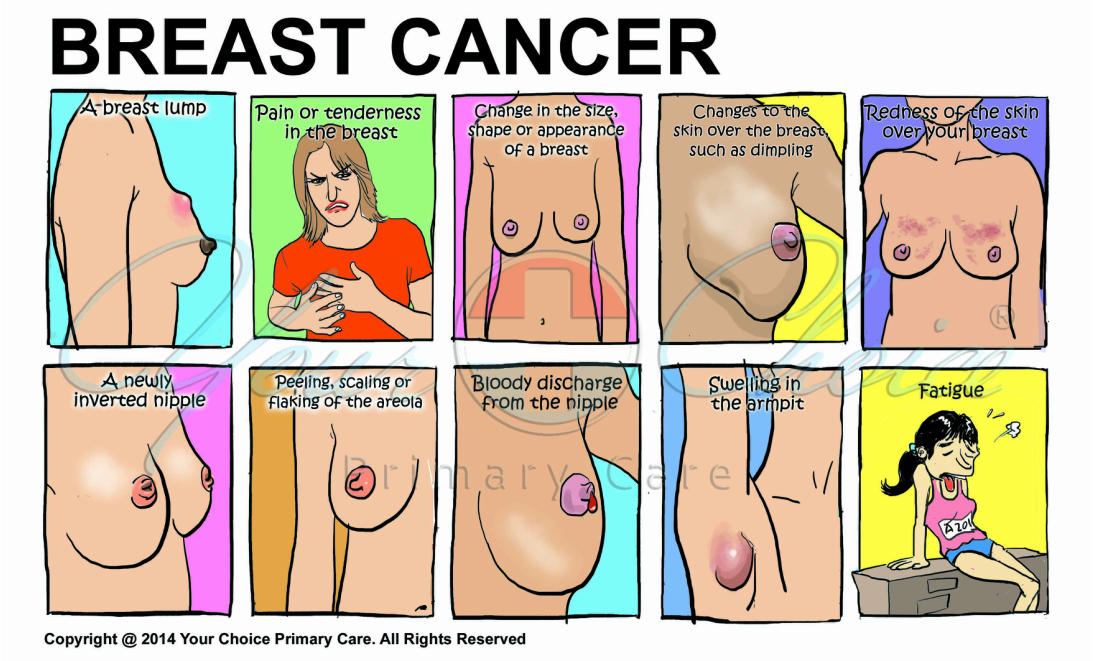
Signs and symptoms of breast cancer may include:
- A breast lump or thickening that feels different from the surrounding tissue
- Bloody discharge from the nipple
- Change in the size, shape or appearance of a breast
- Changes to the skin over the breast, such as dimpling
- A newly inverted nipple
- Peeling, scaling or flaking of the pigmented area of skin surrounding the nipple (areola) or breast skin
- Redness or pitting of the skin over your breast, like the skin of an orange
- Fatigue
When to see a doctor
If you find a lump or other change in your breast — even if a recent mammogram was normal — make an appointment with your primary doctor for prompt evaluation.
Breast cancer occurs when some breast cells begin growing abnormally. These cells divide more rapidly than healthy cells do and continue to accumulate, forming a lump or mass. The cells may spread (metastasize) through your breast to your lymph nodes or to other parts of your body.
Researchers have identified hormonal, lifestyle and environmental factors that may increase your risk of breast cancer.
Doctors estimate that only 5 to 10 percent of breast cancers are linked to gene mutations passed through generations of a family. A number of inherited mutated genes that can increase the likelihood of breast cancer have been identified. The most common are breast cancer gene 1 (BRCA1) and breast cancer gene 2 (BRCA2), both of which significantly increase the risk of both breast and ovarian cancer. Consider asking your doctor for a referral to a genetic counselor, who can review your family health history. A genetic counselor can also discuss the benefits, risks and limitations of genetic testing with you and guide you on appropriate genetic testing.
Factors that are associated with an increased risk of breast cancer include:
- Being female. Women are much more likely than men are to develop breast cancer.
- Increasing age. Your risk of breast cancer increases as you age.
- A personal history of breast cancer. If you've had breast cancer in one breast, you have an increased risk of developing cancer in the other breast.
- A family history of breast cancer. If your mother, sister or daughter was diagnosed with breast cancer, particularly at a young age, your risk of breast cancer is increased. Still, the majority of people diagnosed with breast cancer have no family history of the disease.
- Inherited genes that increase cancer risk. Certain gene mutations that increase the risk of breast cancer can be passed from parents to children. The most common gene mutations are referred to as BRCA1 and BRCA2. These genes can greatly increase your risk of breast cancer and other cancers.
- Radiation exposure. If you received radiation treatments to your chest as a child or young adult, your risk of breast cancer is increased.
- Obesity. Being obese increases your risk of breast cancer.
- Beginning your period at a younger age. Beginning your period before age 12 increases your risk of breast cancer.
- Beginning menopause at an older age. If you began menopause at an older age, you're more likely to develop breast cancer.
- Having your first child at an older age. Women who give birth to their first child after age 35 may have an increased risk of breast cancer.
- Having never been pregnant. Women who have never been pregnant have a greater risk of breast cancer than do women who have had one or more pregnancies.
- Postmenopausal hormone therapy. Women who take hormone therapy medications that combine estrogen and progesterone to treat the signs and symptoms of menopause have an increased risk of breast cancer. The risk of breast cancer decreases when women stop taking these medications.
- Drinking alcohol. Drinking alcohol increases the risk of breast cancer.
Women with breast cancer may have appointments with their primary care doctors as well as several other doctors and other health professionals, including:
- Breast health specialists
- Breast surgeons
- Doctors who specialize in diagnostic tests, such as mammograms (radiologists)
- Doctors who specialize in treating cancer (oncologists)
- Doctors who treat cancer with radiation (radiation oncologists)
- Genetic counselors
- Plastic surgeons
Tests and procedures used to diagnose breast cancer include:
- Breast exam. Your doctor will check both of your breasts and lymph nodes in the armpit, feeling for any lumps or other abnormalities.
- Mammogram. A mammogram is an X-ray of the breast. Mammograms are commonly used to screen for breast cancer. If an abnormality is detected on a screening mammogram, your doctor may recommend a diagnostic mammogram to further evaluate that abnormality.
- Breast ultrasound. Ultrasound uses sound waves to produce images of structures deep within the body. Ultrasound may help distinguish between a solid mass and a fluid-filled cyst. An ultrasound is often obtained as part of the examination of a new lump.
- Removing a sample of breast cells for testing (biopsy). Biopsy samples are sent to a laboratory for analysis where experts determine whether the cells are cancerous. A biopsy sample is also analyzed to determine the type of cells involved in the breast cancer, the aggressiveness (grade) of the cancer, and whether the cancer cells have hormone receptors or other receptors that may influence your treatment options.
- Breast magnetic resonance imaging (MRI). An MRI machine uses a magnet and radio waves to create pictures of the interior of your breast.
Tests and procedures used to stage breast cancer may include:
- Blood tests, such as a complete blood count
- Mammogram of the other breast to look for signs of cancer
- Breast MRI
- Bone scan
- Computerized tomography (CT) scan
- Positron emission tomography (PET) scan
Not all women will need all of these tests and procedures. Your doctor selects the appropriate tests based on your specific circumstances and taking into account new symptoms you may be experiencing. Your doctor determines your breast cancer treatment options based on your type of breast cancer, its stage and grade, size, and whether the cancer cells are sensitive to hormones. Your doctor also considers your overall health and your own preferences. Most women undergo surgery for breast cancer and also receive additional treatment before or after surgery, such as chemotherapy, hormone therapy or radiation.
Breast cancer surgery
- Removing the breast cancer (lumpectomy). During lumpectomy, which may be referred to as breast-sparing surgery or wide local excision, the surgeon removes the tumor and a small margin of surrounding healthy tissue. Lumpectomy is typically reserved for smaller tumors.
- Removing the entire breast (mastectomy). Most mastectomy procedures remove all of the breast tissue — the lobules, ducts, fatty tissue and some skin, including the nipple and areola (simple mastectomy). In a skin-sparing mastectomy, the skin over the breast is left intact to improve reconstruction and appearance. Depending on the location and size of the tumor, the nipple may also be spared.
- Removing a limited number of lymph nodes (sentinel node biopsy). To determine whether cancer has spread to your lymph nodes, your surgeon will discuss with you the role of removing the lymph nodes that are the first to receive the lymph drainage from your tumor. If no cancer is found in those lymph nodes, the chance of finding cancer in any of the remaining lymph nodes is small.
- Removing several lymph nodes (axillary lymph node dissection). If cancer is found in the sentinel node, your surgeon will discuss with you the role of removing additional lymph nodes in your armpit.
- Removing both breasts. Some women with cancer in one breast may choose to have their other (healthy) breast removed if they have a very increased risk of cancer in the other breast because of a genetic predisposition or strong family history.
Radiation therapy uses high-powered beams of energy, such as X-rays, to kill cancer cells. Radiation therapy is typically done using a large machine that aims the energy beams at your body. But radiation can also be done by placing radioactive material inside your body.
Chemotherapy uses drugs to destroy cancer cells. If your cancer has a high risk of returning or spreading to another part of your body, your doctor may recommend chemotherapy to decrease the chance that the cancer will recur. Chemotherapy is sometimes given before surgery in women with larger breast tumors. The goal is to shrink a tumor to a size that makes it easier to remove with surgery. Chemotherapy is also used in women whose cancer has already spread to other parts of the body. Chemotherapy may be recommended to try to control the cancer and decrease any symptoms the cancer is causing.
Hormone therapy — perhaps more properly termed hormone-blocking therapy — is often used to treat breast cancers that are sensitive to hormones. Doctors sometimes refer to these cancers as estrogen receptor positive (ER positive) and progesterone receptor positive (PR positive) cancers. Hormone therapy can be used after surgery or other treatments to decrease the chance of your cancer returning. If the cancer has already spread, hormone therapy may shrink and control it.
Treatments that can be used in hormone therapy include:
- Medications that block hormones from attaching to cancer cells. Selective estrogen receptor modulator (SERM) medications act by blocking estrogen from attaching to the estrogen receptor on the cancer cells, slowing the growth of tumors and killing tumor cells. SERMs include tamoxifen, raloxifene (Evista) and toremifene (Fareston).
Medications that stop the body from making estrogen after menopause. Called aromatase inhibitors, these drugs block the action of an enzyme that converts androgens in the body into estrogen. These drugs are effective only in postmenopausal women. Aromatase inhibitors include anastrozole (Arimidex), letrozole (Femara) and exemestane (Aromasin). - A drug that targets estrogen receptors for destruction. The drug fulvestrant (Faslodex) blocks estrogen receptors on cancer cells and signals to the cell to destroy the receptors. Fulvestrant is used in postmenopausal women.
- Surgery or medications to stop hormone production in the ovaries. In premenopausal women, surgery to remove the ovaries or medications to stop the ovaries from making estrogen can be an effective hormonal treatment.
Targeted drug treatments attack specific abnormalities within cancer cells. Targeted drugs used to treat breast cancer include:
- Trastuzumab (Herceptin). Some breast cancers make excessive amounts of a protein called human growth factor receptor 2 (HER2), which helps breast cancer cells grow and survive. If your breast cancer cells make too much HER2, trastuzumab may help block that protein and cause the cancer cells to die.
- Pertuzumab (Perjeta). Pertuzumab targets HER2 and is approved for use in metastatic breast cancer in combination with trastuzumab and chemotherapy. This combination of treatments is reserved for women who haven't yet received other drug treatments for their cancer.
- Ado-trastuzumab (Kadcyla). This drug combines trastuzumab with a cell-killing drug. When the combination drug enters the body, the trastuzumab helps it find the cancer cells because it is attracted to HER2. The cell-killing drug is then released into the cancer cells. Ado-trastuzumab may be an option for women with metastatic breast cancer who've already tried trastuzumab and chemotherapy.
- Lapatinib (Tykerb). Lapatinib targets HER2 and is approved for use in advanced or metastatic breast cancer. Lapatinib can be used in combination with chemotherapy or hormone therapy.
No alternative medicine treatments have been found to cure breast cancer.
A breast cancer diagnosis can be overwhelming. And just when you're trying to cope with the shock and the fears about your future, you're asked to make important decisions about your treatment. Every woman finds her own way of coping with a breast cancer diagnosis. Until you find what works for you, it might help to:
- Learn what you need to know about your breast cancer. Knowing more about your cancer and your options may help you feel more confident when making treatment decisions. Still, some women may not want to know the details of their cancer. If this is how you feel, let your doctor know that, too.
- Talk with other breast cancer survivors. You may find it helpful and encouraging to talk to other women with breast cancer. Contact the American Cancer Society to find out about support groups in your area and online.
- Find someone to talk about your feelings with. Find a friend or family member who is a good listener, or talk with a clergy member or counselor.
- Keep your friends and family close. Your friends and family can provide a crucial support network for you during your cancer treatment.
Maintain intimacy with your partner. In Western cultures, women's breasts are associated with attractiveness, femininity and sexuality. Because of these attitudes, breast cancer may affect your self-image and erode your confidence in intimate relationships. Talk to your partner about your insecurities and your feelings.
Making changes in your daily life may help reduce your risk of breast cancer.
- Ask your doctor about breast cancer screening. Discuss with your doctor when to begin breast cancer screening exams and tests, such as clinical breast exams and mammograms.
- Become familiar with your breasts through breast self-exam for breast awareness. Women may choose to become familiar with their breasts by occasionally inspecting their breasts during a breast self-exam for breast awareness. If there is a new change, lumps or other unusual signs in your breasts, talk to your doctor promptly.
- Drink alcohol in moderation, if at all. Limit the amount of alcohol you drink to less than one drink a day, if you choose to drink.
- Exercise most days of the week. Aim for at least 30 minutes of exercise on most days of the week.
- Limit postmenopausal hormone therapy. Combination hormone therapy may increase the risk of breast cancer. Talk with your doctor about the benefits and risks of hormone therapy.
- Maintain a healthy weight. If your weight is healthy, work to maintain that weight. If you need to lose weight, ask your doctor about healthy strategies to accomplish this. Reduce the number of calories you eat each day and slowly increase the amount of exercise.
If your doctor has assessed your family history and other factors and determined that you may have an increased risk of breast cancer, options to reduce your risk include:
- Preventive medications (chemoprevention). Estrogen-blocking medications may help reduce the risk of breast cancer. Options include tamoxifen and raloxifene (Evista). Aromatase inhibitors have shown some promise in reducing the risk of breast cancer in women with a high risk. These medications carry a risk of side effects, so doctors reserve these medications for women who have a very high risk of breast cancer.
- Preventive surgery. Women with a very high risk of breast cancer may choose to have their healthy breasts surgically removed. They may also choose to have their healthy ovaries removed to reduce the risk of both breast cancer and ovarian cancer.